Cardiology still a leader in healthcare AI, trailing only radiology in FDA-cleared algorithms
The number of clinical artificial intelligence (AI) algorithms cleared by the U.S. Food and Drug Administration (FDA) is on track to surpass 1,000 before the end of the 2024. Cardiology continues to be the No. 2 speciality with the most AI algorithms, according the FDA's most recent AI update released Aug. 7.
At its current rate, the number of clinical algorithms cleared by the FDA will break 1,000 before the end of 2024. The total sat at 950 as of the end of June. This includes 61 new approvals since the last FDA update from March. Cardiology added 13 new algorithms during that time.
Overall, cardiology now has 135 FDA-cleared AI models, 14.2% of the total number of approved algorithms.
Radiology, which had 44 new approvals since the previous update, accounts for the largest number of AI approvals from the FDA by far. Radiology now makes up about 76% of 950 algorithms cleared so far. The third closest speciality for AI is neurology, with 34 algorithms, or about 3.5% of the AI clearances.
Most of the cardiology AI is concentrated on ECG and image analysis.
AI poised to change how cardiology is practiced
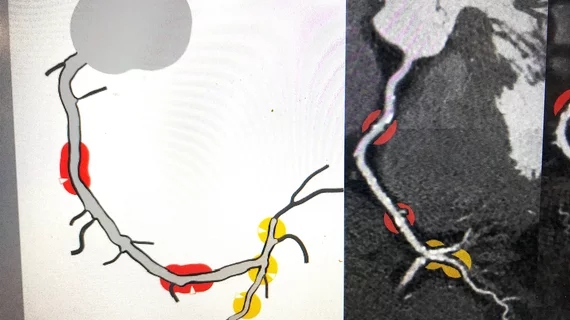
One of the most recently cleared cardiology AI algorithms is HeartFlow's Roadmap Analysis AI. It can analyze cardiac CT results, acting as a second set of eyes and even delivering automated measurements of coronary artery disease stenosis. It creates easier-to-understand, image-based assessments that can then be forwarded to referring physicians and shared with patients to better explain the patient's disease state.
"I use the Roadmap technology in a wide variety of ways. It really helps raise up level-two readers who may not have the experience level-three readers may, but also builds consistency in the reads and decreases the time that it actually takes to read. We use the technology to help train new fellows as well," explained Sarah Jane Rinehart, MD, the director of cardiac imaging at Charleston Area Medical Center, in an interview with Cardiovascular Business.
Another example is the automation found on the Siemens's Origin echocardiography system, which automates hundreds of measurements to help speed exams and reporting. The AI also anticipates next moves in exams and automates strain assessments to make workflows faster and more reproducible,
"AI is crucial for individualizing and personalizing care, as well as enhancing patient engagement," explained Jagmeet Singh, MD, PhD, a leading expert in electrophysiology (EP) and a professor of medicine at Harvard Medical School, who delivered a keynote address on the transformative role of AI in cardiology at the Heart Rhythm Society (HRS) 2024 meeting.
In EP, wearable cardiac monitors are now being used to more easily assess patients, but these devices record data 24 hours a day for the duration of monitoring. In the case of implantable cardiac monitors this could include contact data records for years. This has led to an explosion of data that is difficult for cardiologists or their staff to sort through. It is also not practical to watch this data 24 hours a day for critical events that may be a safety concern for the patient.
"Wearables, I think, will eventually cannibalize implantable devices," Singh predicted. He emphasizing the role of AI in managing and interpreting the vast amount of data generated by these devices to reduce false positives and clinician burnout.
These newer, wearable cardiac monitors under the watch of AI 24/7 has also led to a growing trend of same-day discharges and home monitoring strategies that allow patients to recover in their own homes while still having their telemetry closely monitored remotely.
"This not only makes fiscal sense but also translates into better clinical outcomes," Singh explained.
On a larger, population-based scale, AI has the potential to identify at-risk patients earlier and with greater accuracy, explained Thomas M. Maddox, MD, SM, professor of medicine and vice president of digital products and innovation at BJC HealthCare, Washington University School of Medicine, and a member of the FDA's Digital Health Advisory Committee, in an interview with Cardiovascular Business.
He said this will likely include the use of passive AI screenings of patients outside of clinical settings, using smartphones, toilet seat and bed sensors, may also detect issues and notify the doctor. This is widely expected to help initiate earlier interventions before a disease progresses to being symptomatic and when it is much easier to treat a patient.
He said AI also has the opportunity to help address one of the key causes of burnout: the massive amount of patient data physicians must sort through on a regular basis.
"There is now a tidal wave of data coming in and we're already overwhelmed with the amount of data we have to manage every day. So we're starting to see some really helpful improvements in data management. For example, a lot of people have been talking about generative AI ... there's been several products on the market that are starting to basically become an ambient scribe. So the idea is that you start to record your clinic visits and then that information is fed into a ChatGPT-like generative AI model that can then turn that information into a clinical note," Maddox explained.
As a result, he said cardiologists get a better chance look patients in the eye and make a real connection instead of being distracted by other things.
The full list of the FDA’s cleared AI-enabled devices can be found here.