7 ways cath labs can work through the contrast media shortage without delays
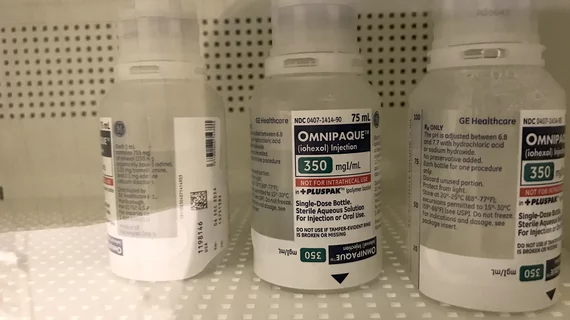
The ongoing contrast media shortage has hit health systems in the United States like a wrecking ball, causing important imaging examinations to be postponed throughout the country.
One prominent system in Ohio, however, responded to the shortage with a pledge not to delay a single cardiac catheterization procedure. Representatives from that system wrote about their decision for JACC: Cardiovascular Interventions, noting that recent experiences with COVID-19 taught them some important lessons.
“The decision was based on a large body of evidence suggesting deleterious consequences of delaying coronary procedures early during the COVID-19 pandemic, when there was a shortage of personal protective equipment,” wrote first author Farshad Forouzandeh, MD, PhD, a specialist with the University Hospitals Harrington Heart and Vascular Institute in Cleveland, and colleagues. “The delay in patient care resulted in late presentation of many patients with a variety of cardiovascular conditions, leading to poor outcomes.”
Forouzandeh et al. wrote that they worked closely with their University Hospitals colleagues to decrease the use of contrast whenever possible. If an alternative testing strategy can accomplish the same goal, they embraced that alternative, saving contrast use for instances when it was truly necessary.
The group also implemented a guideline for the system’s cath labs. That guideline focused on seven key recommendations for labs looking to safely reduce contrast without delaying patient care:
- Shift from automated contrast injection systems to manifold, except for transcatheter aortic valve replacement (TAVR) procedures.
- Consolidate diagnostic cases to a single operator whenever possible.
- Consider “more definitive testing” in the cath lab to minimize contrast angiography.
- Limit optical coherence tomography, using intravascular ultrasound for guidance when needed.
- Closely monitor the amount of contrast being used at all times.
- Consider CO2 angiography and IVUS for peripheral procedures.
- Redistribute contrast to smaller vials to help keep waste to a minimum.
This guideline was shared throughout the system on May 10, 2022. To test its effectiveness, the authors compared data from the two weeks before the guideline was finalized to the two weeks after the guideline.
Overall, the group found, their guideline helped reduce the average contrast used per cath lab procedure by nearly 46%.
“Of note, our structural team has switched from contrast-enhanced computed tomographic angiography to noncontrast computed tomography with or without magnetic resonance angiography for access-site evaluation, leading to more contrast preservation before the TAVR procedures,” the authors wrote.
The team concluded that its guideline for cath labs was such a success that it will likely continue “many aspects” once the shortage is a thing of the past.
Related Contrast Shortage Content:
VIDEO: Mitigating the contrast media shortage impact on CT imaging
VIDEO: American College of Radiology working with FDA to mitigate contrast shortage
VIDEO: How the iodine contrast shortage is impacting interventional cath labs
Gadolinium can be used as substitute for iodine contrast in some interventional imaging procedures
Reference: