Q&A: William Zoghbi breaks down the future of echocardiography
Ultrasound is the most widely used cardiac imaging modality and it has witnessed several advances in recent years that are making echocardiography more accessible, accurate and efficient. Advances in computer processing have also made a quantum jump in the past decade, allowing much more of the data collected by ultrasound to be processed and presented in a usable format to bolster patient care.
Cardiovascular Business discussed these recent trends with William A. Zoghbi, MD, MACC, FAHA, FASE, chair of the Department of Cardiology at Houston Methodist DeBakey Heart and Vascular Center, and past president of both the American College of Cardiology (ACC) and the American Society of Echocardiography (ASE). He also was the course director for the ASE State-of-the-Art Echocardiography 2022 course that took place in late February, which
Zoghbi said the top 5 cardiac ultrasound trends include:
• Artificial Intelligence (AI)
• Strain imaging
• 3D echo systems
• Point of care ultrasound systems (POCUS)
• Structural heart interventions, and
• The impact of COVID-19 on ultrasound
Watch the VIDEO: New Advances in Echocardiography — Interview with William A. Zoghbi, MD
What do you see as the key technology advances in echo?
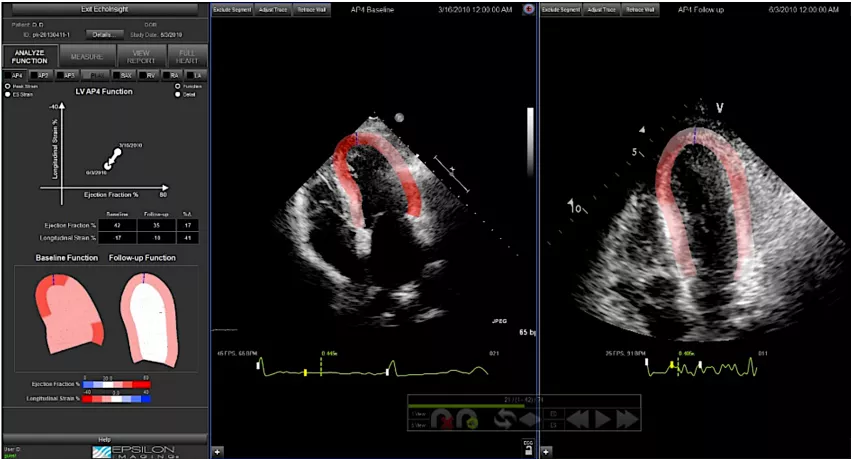
William Zoghbi: Well, actually the field of echo has never been stagnant. And I think this year has not been any different, with some very exciting, newer aspects of ultrasound. The basics of ultrasound have not changed, but what has changed is how do you process this, and what kind of information do you get. You hear about the use of strain for the left ventricle and global longitudinal strain, but also there is use of strain for the assessment of the right ventricle and left atrial function. This improves our diastolic function assessment in patients such as those with heart failure and patients with shortness of breath. The right ventricle has always been more problematic for echocardiography, so having this technology to assess the right ventricle function, is really a significant advancement.
Have you seen a wider adoption of myocardial strain in recent years? This was a pretty hot topic at the 2019 ASE meeting.
William Zoghbi: I think there is much more adoption now. People are much more comfortable with it. The technology is better now, more robust. There is still a little bit of variability among vendors, but overall, adoption is much better than before. People are using it to compliment their overall interpretation of the echocardiograms.
I think it also can help use with the ventricle to look for certain patterns that alert us to infiltrative diseases like amyloidosis. Nowadays, amyloidosis has a treatment as opposed to the past. So I think having this in our armamentarium will certainly help us navigate and help patients in much better ways.
AI for cardiac ultrasound has now been commercialized. How is this helping cardiology?
William Zoghbi: I think the big excitement right now is the applications of AI and machine learning. For example, AI can enhance the accuracy of acquiring images. In echocardiography, as opposed to other technologies, it is the individual who is acquiring the images with the transducer in their hand that can influence the adequacy of the images, and therefore the interpretation. So nowadays, with AI, it can give you a signal while you're acquiring these images as to whether they're appropriate and in the best format for different views of the parasternal long axis or the apical views of the heart.
And the amazing thing is that these are available now in portable ultrasound, and even the handheld devices that can really help you at the bedside wherever you are. And they've been tested in individuals who have not had significant training before. I think that is very helpful.
On the display and interpretation side, meanwhile, I think the echocardiography field is gradually moving toward enhancing the display of various images since they can be obtained in multiple fashions, to put them together in a way to enhance the interpreter. For example, if you want to look at the left ventricle, the machine would recognize all the acquired images would know these are to emphasize the left ventricle. So you have all the views that relate to the left ventricle. If you want to assess the right ventricle, if you assess aortic valve or the mitral valve, I think this is where the field is going to give you as much information as an interpreting physician to collate all these, and come up with a better, and hopefully more accurate diagnosis.
The third trend I'm seeing in AI is automation. The automation of measurements, of ventricular volumes, of ejection fraction, of 3D volumes, you will see quite a bit of that. The field needed something like this to enhance the process and basically put all these various parameters that may be quite complex at the fingertips of the interpreting physician. So I think that this is a significant advance for echocardiography.
One of our international attendees in the ASE program last week said they can't wait for AI to be implemented in our world because it brings all the technology and knowledge to our fingertips.
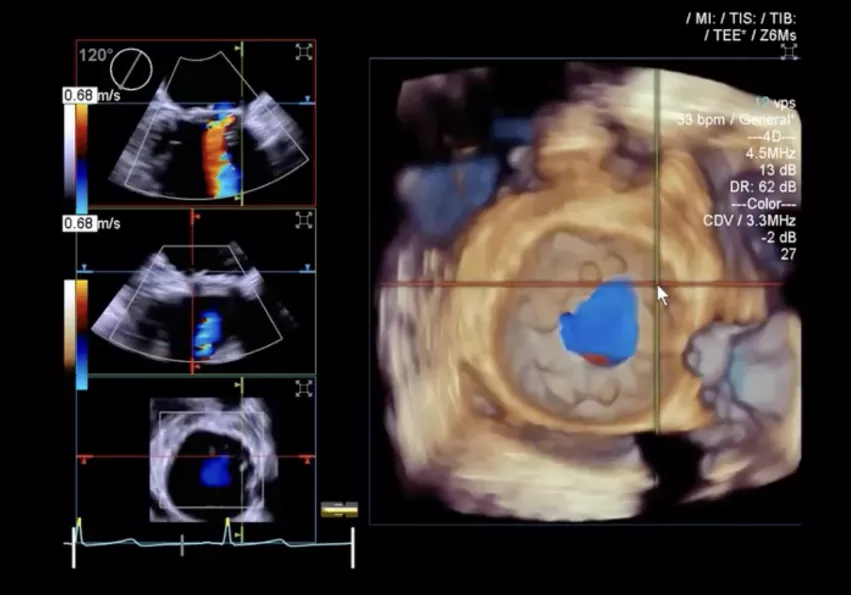
There appears to be a much wider adoption of 3D echo acquisition systems over the past few years. Is this a trend that you've been seeing?
William Zoghbi: I think you will see the majority of systems nowadays already have 3D incorporated in them. What we need there is more educational formats. But I think 3D is going to be very important in certain situations. One situation where it really matters is if you have somebody with a lot of regional abnormalities of the heart, previous infractions, etc., this is where the estimation of an ejection fraction or volumes may be difficult. The impact of 3D echo could be felt the most in these situations where accuracy becomes more difficult. It will be very helpful for us.
In valvular heart disease, obviously 3D with transesophageal echo has been crucial for mitral valve disease, particularly in visualizing in real time the various scallops of the mitral valve and where the abnormalities are.
Structural heart has become a big focus of echo. What are some advances in echo that are helping improve workflow?
William Zoghbi: When we talk about structural heart, we emphasize mostly valvular heart disease, but there are also the occluder devices that interventional cardiologists use, be it inter-atrial septum or left atrial appendage. But for valvular heart disease, a really big focus nowadays is really much more on the mitral valve, and particularly the tricuspid valve. These have been areas where people have not focused as much in the past, because obviously it's a little more challenging. But nowadays, I think we have the technology to be able to help in pre-procedural evaluation when it comes guiding the interventional cardiologist for the assessment of regurgitation and severity of stenosis. I think the role of an interventional imager nowadays is particularly on the mitral and tricuspid disease.
In the aortic realm, I think most institutions nowadays are using a quick transthoracic examination during the procedure. So we feel less of an urgent need to do a transesophageal, unless you have an unusual situation or maybe complications. But I think it is crucial for the use of echo to guide the procedure. You need an interventional imager who is very adapt in acquiring the images and interacting with the interventional cardiologists to see the deployment of either a repair clip or a total valve deployment. And I think you're going to see this grow tremendously in the near future.
What are the impacts of these technologies in terms of helping patients or aiding workflow?
William Zoghbi: We have more and more information that is coming from the usual echocardiographic examination. I think if you compare what we were doing 20 years ago, 15 years ago, to what we're doing now, the information that you're getting from the same examination is so much more. To serve patients well, you have to look at structure, function, diastolic assessment, and everything else, and all that takes time. So most often, patients are scheduled for almost an hour examination or so. Yes, you can cut it down a bit, but you don't want to short change getting as much the information that is needed. The beauty of ultrasound is it is very versatile and can be taken to the bedside, and this is where it's implications are.
Everybody is cognizant of the value of their time. But if it helps you make a quick diagnosis at the bedside to initiate therapy.
What has the impact of COVID-19 been on echocardiography?
William Zoghbi: During the early phases of the pandemic, echo was impacted in two ways. One, there was lesser utilization early on where we had to be cognizant of what to do and how to do it. But at the same time, there was much more stress on the echocardiography field because it is a technology that is available at the bedside. So therefore the sonographers were on the front line. Really my hat is off to our sonographers throughout the nation and the world. Early on during the pandemic, we were not doing stress testing. We took patients to the catheterization laboratory only if they were unstable or were unusual, but all the diagnostics on heart failure, and the shortness of breath, and understanding the heart function, and the right ventricular function that was affected so much because of the COVID pulmonary disease, that actually increased utilization of echocardiography. We are still doing that because we've had four or five phases of this pandemic come through.
But currently I think we're close to back to where we were prior to COVID when it comes to utilization. Or maybe utilization is up a bit. Patients are much more comfortable with the precautions that we use and everything else.
Point-of-care ultrasound (POCUS) appears to have exploded over the last two years due to COVID. Are you still seeing this?
William Zoghbi: The portability is one of the advantages of echocardiography, and there are even handheld devices that you could now use. But there are some other things to remember as well. One is that, in difficult patients who are attached to a lot of instrumentation, very short of breath or really critically ill, you have to be cognizant of the limitations of such miniaturized devices. They may still give you the information you need, but you don't want to shortchange the patient. If you are really unsure about what you see, you really want a full examination with a more powerful instrument. There's no question about it. Two, I think we have to be cognizant of difficult patients. With these people who are more difficult to interpret, you may need the full power of a larger ultrasound system. And what I mean by that is good Doppler, spectral, CW, color, good penetration.
I'm not downgrading the importance of smaller, portable systems; I think they are going to be very important in our bedside management of critically ill patients. But my message is, if you're not satisfied with what you get, and if you're not satisfied with interpretation and overall diagnosis of such a patient, I would not hesitate to bring in a more powerful machine.
VIDEO: New Advances in Echocardiography — Interview with William A. Zoghbi, MD
Find more news on cardiac ultrasound
Related Content With William Zoghbi:
ACC Corner: Let’s be ’CardioSmart’ - by William Zoghbi
Choosing Wisely: Beyond the Low Hanging Fruit - by William Zoghbi
Seeing the Big Picture: Training Today’s Imagers to ‘Think Multimodality’