ASE shares new guidelines for ultrasound-guided vascular access
The American Society of Echocardiography (ASE) has published new guidelines for ultrasound-guided vascular cannulation, which has seen considerable growth over the past decade due to its safety benefits.
Guidelines for Performing Ultrasound-Guided Vascular Cannulation: Recommendations of the ASE was published in the Journal of the American Society of Echocardiography.[1] It replaces ASE's original guideline from 2011. The new document provides expert consensus on the best practices and techniques for using ultrasound in vascular access procedures.
A decade ago, anatomical landmarks were used to find the approximate location when inserting a needle to gain catheter access to arteries and veins for cath lab-based procedures. But a growing number of centers since then have adopted point-of-care ultrasound (POCUS) systems to visualize needle guidance and help avoid vascular complications. It has become and essential skill across various cardiovascular ultrasound specialties during diagnostic and medical procedures. Dedicated vascular access POCUS systems are now commonly found in many cath labs.
“Ultrasound guidance is currently not a standard-of-care for all vascular access, but it is becoming increasingly common in daily clinical practice due to its ability to enhance success rates and reduce complications,” lead co-author Annette Vegas, MDCM, an anesthesiologist and director of peri-operative echocardiography at Toronto General Hospital in Ontario, Canada, in a statement. “Adopting the recommendations in this guideline will help clinicians better minimize risks, maximize technical competencies and ultimately, improve patient outcomes.”
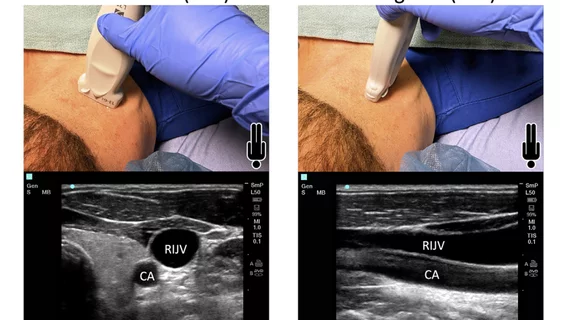
ASE said the new guideline uses descriptions, diagrams and ultrasound images to explain the general aspects of the anatomy and ultrasound imaging of vessels, vascular cannulation techniques, and the identification of vascular complications.
The key areas discussed in the guideline include precannulation vessel assessment, dynamic ultrasound guidance and the identification of local complications.
There are venous access sections specific to the internal jugular, subclavian, axillary and common femoral veins. Arterial cannulation details are included for the radial, ulnar, brachial axillary, carotid, common femoral, posterior tibial, dorsalis pedis and issues specific to pediatric vascular access.
The guidelines also highlights how to identify complications, including hematoma, abscess, seroma, lymphocele, thrombosis, stenosis, vasospasm and major bleeding events. In addition, it covers arterial cannulation complications such as arterial dissection, pseudoaneurysm and arteriovenous fistula, and issues related to damaging surrounding structures, such as the lungs, nerves or lymphatics.