Ultrafast myocardial contrast echocardiography shows early potential to evaluate CAD
Ultrafast myocardial contrast echocardiography (MCE) can accurately evaluate myocardial ischemia in patients with suspected obstructive coronary artery disease (CAD), according to the world’s first study to compare the new modality to traditional MCE in humans.
Sharing their findings in Circulation: Cardiovascular Imaging, the study’s authors suggested ultrafast MCE showed potential to eventually be a go-to imaging option for cardiologists.
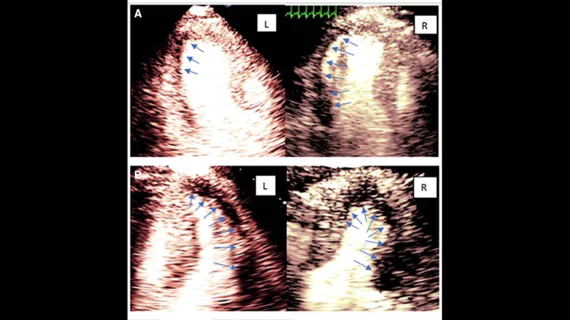
“Clinical MCE utilizes commercial microbubbles for myocardial perfusion assessment for the detection of obstructive OCAD,” wrote first author Lasha Gvinianidze, MD, a cardiologist with London Northwest University Healthcare in the United Kingdom, and colleagues. “However, its accuracy is limited by the image quality … High frame rate or ultrafast ultrasound MCE, due to its high temporal resolution, can reduce noise and minimize motion artifacts, thus improving perfusion assessment as demonstrated in healthy volunteers.”
To learn more, Gvinianidze et al. performed a first-in-human study that examined 25 patients who underwent rest and vasodilator perfusion imaging using both conventional cardiac ultrasound and ultrafast techniques. The ultrafast MCE was performed using Verasonics Vantage technology. The mean patient age was 64 years old, and 72% were men.
Overall, the modalities were comparable when it came to identifying patients with obstructive CAD, but ultrafast MCE identified more segments with inducible perfusion defects. Also, where conventional MCE identified mild defects, the ultrafast MCE identified severe defects.
“In this first study in humans with obstructive CAD, high frame rate MCE, despite using a research platform without optimization and without using a detailed data processing algorithm unlike conventional MCE, is as accurate for the detection of obstructive CAD,” the authors wrote. “However, high frame rate MCE detected larger and more severe ischemic burden, which has diagnostic and prognostic implications even in the absence of obstructive CAD.”
If this technology can be studied more and “established through larger trials,” they concluded, it “may well become the initial functional test for the assessment of obstructive CAD.”