USPSTF highlights the benefits of statin use among high-risk CVD patients in new recommendations
The U.S. Preventive Services Task Force (USPSTF) has finalized its new recommendations on the use of statins to prevent cardiovascular disease (CVD). The group first shared a draft of these recommendations in February, leaving them open for public comment until March 22.
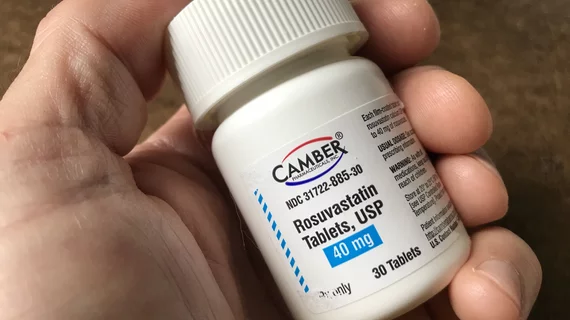
The USPSTF recommends statin use for high-risk patients between the ages of 40 to 75 to help prevent a first heart attack or stroke. This received the group’s “B” recommendation, which means “there is high certainty that the net benefit is moderate, or there is moderate certainty that the net benefit is moderate to substantial.”
Patients from this same age group who face an elevated risk of CVD—not a high risk—could still potentially benefit from statin use, the USPSTF said. This received the group’s “C” recommendation, which means it should be offered to patients based on “professional judgment and patient preferences.”
When it comes to statin use among patients 76 years old and older, the USPSTF said it could not make a recommendation at this time. This received the group’s “I” recommendation, which means the current evidence is “insufficient to assess the balance of benefits and harms.”
“Statins effectively and safely prevent first heart attacks and strokes for some people,” John Wong, MD, USPSTF member and interim chief scientific officer at Tufts Medical Center in Boston, said in a prepared statement. “Whether someone should start taking a statin depends on their age and their risk for having a first heart attack or stroke.”
The group also used its final recommendation to emphasize the continued presence of inequities in patient access to statins. Hispanic patients in the United States use statins much less than other races and ethnicities, according to the USPSTF, followed by Asian and Black patients.
“It is essential that we work to better understand the causes of these inequities and reverse the negative impacts of systemic racism on cardiovascular health,” Katrina Donahue, MD, USPSTF member and professor and vice chair of research at the University of North Carolina at Chapel Hill Department of Family Medicine, said in the group’s statement.