Robotic aortic valve replacement may offer certain benefits over TAVR
Using advanced robotics to guide surgical aortic valve replacement (SAVR) procedures may be a safe and effective alternative to transcatheter aortic valve replacement (TAVR) in low- and intermediate-risk patients with severe aortic stenosis (AS), according to a new analysis published in The Annals of Thoracic Surgery.[1]
“Robotic aortic valve replacement (RAVR) is a recently developed minimally invasive surgical strategy with multicenter reproducibility,” wrote first author Vikrant Jagadeesan, MD, an assistant professor with the department of cardiovascular and thoracic surgery at West Virginia University School of Medicine, and colleagues. “In contrast to other minimally invasive SAVR approaches, this sternal and major muscle sparing method permits use of standard surgical valves while also providing the opportunity for performance of concomitant procedures. Therefore, the purpose of this study was to compare a propensity-matched cohort of patients undergoing RAVR versus TAVR for symptomatic severe AS and evaluate perioperative as well as one-year endpoints.”
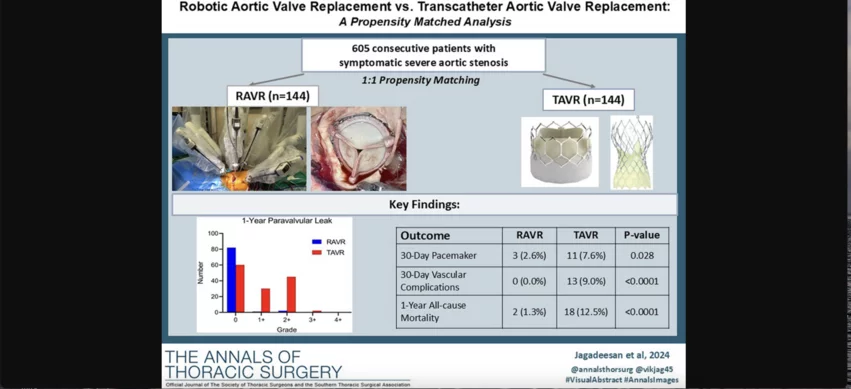
Jagadeesan et al. explored data from 144 patients who underwent RAVR and another 144 who underwent TAVR. Propensity matching was based on Society of Thoracic Surgeons (STS) predicted risk of mortality and valve pathology. All patients were managed by the same heart team at a high-volume academic referral center from 2017 to 2023. Specialists confirmed eligibility for RAVR through the use of extensive CT imaging. Mean patient ages were 69 years old for the RAVR group and 70 years old for the TAVR group. Meanwhile, 63.2% of patients in the RAVR group and 55.6% of patients in the TAVR group were men.
RAVR procedures involved a Da Vinci Xi robot from California-based Intuitive Surgical. Concomitant procedures such as left atrial appendage obliteration and mitral valve repair or replacement were performed on 19% of RAVR patients.
Overall, there were no differences in in-hospital or 30-day mortality between the two groups. Sternotomy was required during two TAVR procedures—once due to cardiac arrest and once due to coronary occlusion—but not at all during RAVR. TAVR was also linked to significantly higher rates of permanent pacemaker implantation (7.6% vs. 2.1%), vascular complications (9% vs. 0%) and stroke events (4.2% vs. 0.7%) than RAVR.
Researchers also found that TAVR patients were much more likely to present with New York Heart Association class III or IV heart failure symptoms or paravalvular leak (PVL) 30 days after treatment than RAVR patients.
A full year later, mean valvular gradients were comparable between the two groups. However, the rates of one-year mortality (12.5% vs. 1.4%) and PVL greater than mild (32.6% vs. 2.3%) were significantly higher among TAVR patients. The group did add that 22% of deaths after TAVR were from cardiac causes and not related to the devices themselves.
“These data enrich the ongoing discussion of the optimal approach to aortic valve replacement in the low to intermediate risk patient with symptomatic severe AS,” the authors wrote. “As enthusiasm behind a 'TAVR for all' approach continues to grow, the multidisciplinary heart team must continue to re-evaluate the evidence base of management alternatives as we incorporate information from highly select randomized TAVR clinical trials.”
The differences in PVL after valve replacement stood out to researchers as an especially significant finding.
“PVL remains a germane consideration in the management of the lower risk patient, and RAVR in this context may provide a viable alternative to mitigate PVL and its potential impact on longitudinal patient outcomes,” they wrote.
Jagadeesan and colleagues did highlight certain limitations with their work, including its retrospective nature and relatively short follow-up times. RAVR is still rare, they added, which is an important point to remember when reviewing these data.
“As RAVR was institutionally initiated, it remains early in its global adoption with less than 30 programs around the world now performing RAVR,” the authors wrote. “Thus, given the relative novelty of RAVR, the study may not yet be widely generalizable.”
Even with these limitations in mind, the group concluded that these findings suggest RAVR may offer care teams a “safe and effective minimally invasive alternative to TAVR” for certain low- and intermediate-risk patients.
Click here to read the full analysis in The Annals of Thoracic Surgery, an STS journal.