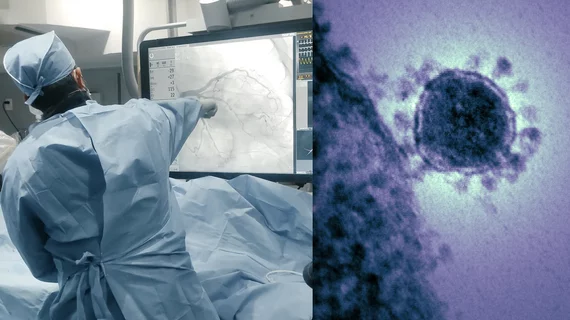
How the availability of vaccines impacted outcomes among STEMI patients with COVID-19
New results from the North American COVID-19 STEMI (NACMI) registry reported a 25% reduction in early mortality in 2021 compared to 2020 among patients with ST-segment elevation myocardial infarction (STEMI) and COVID-19 infection and zero deaths for patients vaccinated against SARS-CoV-2. The data was presented as a late-breaking study Monday at ACC.22, the American College of Cardiology’s 71st Annual Scientific Session and Expo.
The NACMI registry is a collaboration between Society for Cardiovascular Angiography and Interventions (SCAI), ACC and Canadian Association of Interventional Cardiology (CAIC). The registry was established in 2020 with to define baseline characteristics and management strategies and outcome data for COVID-positive patients presenting with STEMI. Sixty-four medical centers across North America and Canada contributed data to the registry. In the initial findings, it was reported that 33% of North American patients with both COVID-19 and a STEMI died in the hospital.
"We noticed early on in the pandemic significant changes in STEMI care and we were trying to understand how COVID was effecting these patients, so that was our motivation for the registry," explained Santiago Garcia, MD, lead author of the study and director of the structural heart program at The Christ Hospital in Cincinnati, Ohio. "We wanted to understand that management strategies and outcomes in the patients, who have really unique high-risk characteristics, including extremely high in-hospital mortality, with one in three patients dying in the hospital."
Patients in 2020 who were positive for COVID-19 and had experienced a STEMI were compared with patients treated in 2021 who had received a COVID-19 vaccine.
In the study, 586 patients were examined, including 227 who were treated in 2020 before vaccinations were made available and 359 in 2021 after multiple vaccines had received emergency use authorization from the FDA. Of the patient population, more than 70% were male and nearly 75% were aged 55 and over. Close to 70% had high blood pressure and nearly 45% were diabetic. Compared to 2020, the proportion of white patients was higher, and patients presented more frequently with typical ischemic symptoms.
When looking at outcomes in 2021, the research team found that survival was significantly better when compared to 2020 with mortality dropping from 33% in 2020 to 23% in 2021. Also, patients treated in 2021 who were vaccinated were less likely to experience sever respiratory illness, and there were no hospital deaths among the population, while patients were unvaccinated experienced a death rate at 22%.
Demographics for patients also changed between 2020 and 2021.
"We have seen significant changes in the patient profiles," Garcia said. "In the first wave of patients we treated in 2020, there was a preponderance of ethnic minorities of about 50%, which is rare for a North American STEMI registry. In 2021, the face of the STEMI patient was different with the majority being Caucasians who are less likely to present with respiratory symptoms and were more likely to present with the usual ischemic symptoms."
He said this change was not arbitrary, it was caused by increasing numbers of people getting the COVID vaccine.
"For those patients who were vaccinated, in-hospital mortality was zero. Whereas mortality for unvaccinated patients remained quite high at 22%," he said. "The message again is the importance of vaccines and how they can prevent the most severe presentations of the disease."
Of those who died, he said the biggest drivers for deaths included how severe the respiratory issues related to COVID were, if a patient was on a ventilator or was in shock.
"Many of these patients die from the co-morbidity related to the lung disease," Garcia said.
“NACMI is a unique collaboration between the SCAI, ACC, and CAIC that has allowed us to develop the largest registry of STEMI in patients with COVID-19 in the world,” said Timothy D. Henry, MD, president of SCAI and study chair. “The unique insights from NACMI enable us to improve care for these high-risk patients.”
Learn more in the VIDEO: Vaccines impacted mortality in COVID STEMI patients and demographics changed — Interview with Santiago Garcia, MD
Related ACC.22 Content:
Links to all the ACC 2022 late-breaking clinical trials
TAVR vs. surgery, FFR-guided PCI and DCB safety: Day 3 at ACC.22
Cholesterol medications, flu shots and heart failure: Day 2 at ACC.22
Salt restrictions, PCI breakthroughs and a social media primer for cardiologists: Day 1 at ACC.22