Implantable Barostim device improves long-term heart failure symptoms
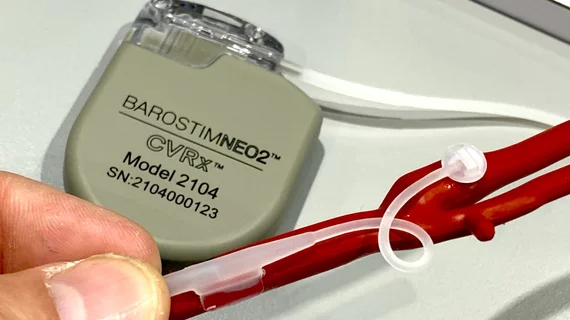
An implantable device that sends electrical pulses to the carotid artery is associated with long-term quality-of-life (QOL) improvements in heart failure patients, according to new findings published in JACC: Heart Failure.[1]
The BeAT-HF trial tracked data from more than 200 heart failure patients, including 124 who underwent baroreflex activation therapy (BAT) with the Barostim device developed by CVRx. The study’s remaining patients served as its control arm, only undergoing guideline-directed medical therapy (GDMT) to treat their symptoms.
Barostim works by sending small electrical pulses to certain baroreceptors in the neck, which then send signals to the brain to help regulate the patient’s heart, kidneys and vascular system. These signals are typically sent without therapy, but this function is diminished in heart failure patients, leading to significant health risks. Barostim has gained both U.S. Food and Drug Administration and CE mark approval, and CMS recently increased the impatient payment for using the device.
Overall, after two years of treatment, Minnesota Living With Heart Failure (MLWHF) Questionnaire scores showed that the BAT group was associated with significant improvements in both their mental and physical QOL. BAT patients were specifically quicker to “return to usual activities,” for example, and experienced greater reductions in reported pain/discomfort.
“Collectively, these results further highlight that patients report a desirable and durable benefit from adding BAT to the standard of care with significant heart failure-specific QOL and general QOL benefits at 24 months,” wrote lead author Samuel F. Sears, PhD, a professor with East Carolina University, and colleagues. “These results are particularly important as BAT is considered for New York Heart Association functional class II/III patients on GDMT and seeking functional improvement in day-to-day activities, improved sleep, and reduced fatigue.”
“To see QOL results that remain this significant in long-term data are rare,” Philip Adamson, MD, chief medical officer of CVRx, said in a statement highlighting the findings. “We believe this analysis of the long-term BeAT-HF data will support the shared decision making of patients and physicians when considering Barostim therapy.”
Click here to read the full research letter in JACC: Heart Failure, an American College of Cardiology journal.
This analysis was funded by CVRx, and multiple authors reported ongoing relationships with CVRx.