Patients with type 2 diabetes and heart disease may require more aggressive, modern treatments
Treating coronary artery disease (CAD) in patients with type 2 diabetes (T2D) may require a more aggressive treatment approach than normal, according to a new scientific statement from the American Heart Association (AHA).
The document, published in full in Circulation, was written by Suzanne V. Arnold, MD, a cardiologist at Saint Luke’s Mid America Heart Institute in Kansas City, Missouri, and several colleagues. It was developed on behalf of the AHA’s Council on Lifestyle and Cardiometabolic Health and Council on Clinical Cardiology.
“What we’ve learned in the past decade is how you control glucose levels has a huge influence on cardiovascular risk,” Arnold said in a statement. “Lowering blood sugars to a certain level is not sufficient. There are now more options for controlling glucose in people with T2D, and each patient should be evaluated for their personal risk of cardiovascular disease, stroke and kidney disease. This combined health information, as well as the patient’s age, should be used to determine the appropriate therapies to lower glucose.”
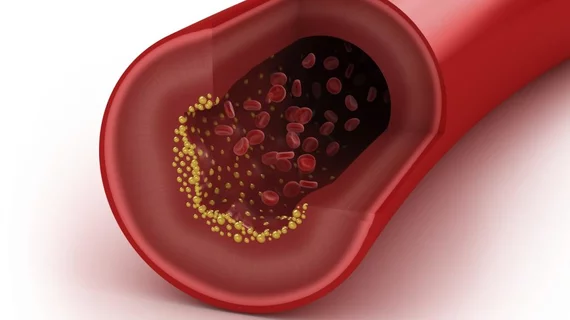
People with T2D are often at an increased risk of developing cardiovascular disease. Their bodies can’t properly control their glucose levels, which can lead to obesity, high blood pressure and high cholesterol. According to Arnold et al., metformin is a typical, affordable medication for individuals with T2D—but other medications show potential to lower glucose and reduce the risk of cardiovascular disease at the same time.
Sodium-glucose co-transporter inhibitors (SGLT2 inhibitors) and glucagon-like peptide-1 receptor agonists (GLP-1 receptor agonists) are two examples of medications that can be used to treat both CAD and T2D. In older patients, there is the additional concern of reducing the risk of hypoglycemia—and this may change the plan of attack with those patients.
“Hypoglycemia is incredibly hard on the heart and should be avoided particularly in older patients,” Arnold said in the same statement. “We must ensure that we are weighing all of the options in consideration of the whole patient, keeping in mind that what may be appropriate for a 60-70 year old patient is likely not the same as for an 85-year old.”
The team also addressed the fact that taking a daily aspirin to prevent blood clots may not be effective for patients with CAD.
“Therefore, newer, stronger antiplatelet medications (a form of blood thinner) should be considered,” Arnold said. “Since all antiplatelet medications increase the risk of bleeding, it is important to balance the risk for each patient of increased bleeding versus the benefit of reducing the tendency of the blood to clot.”
One other key detail is that coronary artery bypass graft (CABG) surgery may be a smarter treatment option for opening arteries to increase blood flow in patients with both CAD and T2D. When patients don’t also have T2D, “the advantage of bypass over stenting is not as dramatic,” according to the AMA statement.