TCT.18: Ultrasound-based renal denervation tops radiofrequency ablation for BP lowering
SAN DIEGO — An endovascular ultrasound-based renal denervation (RDN) approach led to greater reductions in blood pressure than radiofrequency ablation in patients with resistant hypertension, according to the first randomized trial to compare the techniques.
The RADIOSOUND-HTN trial, presented Sept. 25 at the Transcatheter Cardiovascular Therapeutics (TCT) meeting and published simultaneously in Circulation, randomized 117 patients 1:1:1 to either radiofrequency RDN of the main renal arteries; radiofrequency RDN of the main arteries, side branches and accessories; or endovascular ultrasound-based RDN of the main renal arteries only.
Participants were 64 years old on average with mean daytime blood pressure of 153/86 mm Hg. They were taking an average of five antihypertensive medications at baseline and weren’t allowed to change their drug regimens unless clinically indicated.
Patients in each group experienced significant drops in daytime ambulatory blood pressure three months after their respective procedures. However, patients in the ultrasound RDN arm had significantly greater reductions than those who had radiofrequency ablation in the main renal artery (13.2/7.6 mm Hg versus 6.5/3.2 mm Hg). Radiofrequency RDN including side branches and accessories fell in the middle in terms of BP reductions—a mean 8.3/6.1 mm Hg drop—but those improvements weren’t statistically significant when compared to radiofrequency RDN of the main artery alone.
“Ultrasound-based ablation of the main renal arteries seems to be superior to multipolar radiofrequency ablation of the main renal arteries,” wrote principal investigator Philipp Lurz, MD, PhD, and colleagues from Heart Center Leipzig at the University of Leipzig in Germany. “The benefit from additional radiofrequency-based ablation of the renal artery’s side branches over ablation of the main renal artery remains undetermined.”
Lurz noted about one billion people worldwide have hypertension—and up to one-third of them have uncontrolled hypertension despite taking medications. The authors said their trial wasn’t designed to determine which elements of the techniques contributed to differences in blood pressure reductions, but they ventured some guesses nonetheless.
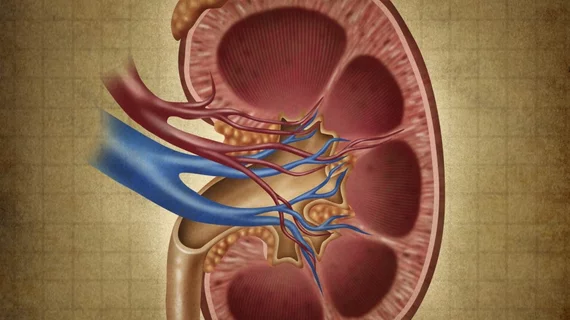
“The use of a balloon-cooled ultrasound catheter has been shown to lead to improved tissue penetration of 6-7 mm from the lumen, affecting up to 90 percent of sympathetic nerve fibers in contrast to the 3-4 mm that can be achieved by radiofrequency catheters,” Lurz and colleagues wrote. “In addition, the device and technology ensure full circumferential ablations. … Although not directly assessed in our study, it seems reasonable that the observed stronger BP reduction could be attributed to an improved treatment depth and/or full circumferential ablation.”
The authors suggested future studies focus on proper patient selection for RDN, as well as determining anatomic predictors of “a more effective RDN procedure.”
“Longer follow-up and larger multicenter studies are needed to do head-to-head comparisons, especially to determine the long-term safety of these technologies,” Lurz said.
Considering these RDN devices are investigational only and not approved for commercial use, cardiologists at a TCT press conference expressed cautious optimism with the results. Larger-scale, sham-controlled trials are ongoing and could further illuminate whether renal denervation therapies warrant a place in routine clinical practice, they said.
“I think there’s good reason to be enthusiastic to investigate,” said Deepak L. Bhatt, MD, MPH, executive director of interventional cardiovascular programs at Brigham and Women’s Hospital in Boston and professor of medicine at Harvard Medical School. “I think it’s interesting that the ultrasound-based catheter appears to be better than radiofrequency ablation, so I think we need to learn a lot more about the technique. I think we need to learn still a lot more about the right patients, but I think we still need more data for powered, sham-controlled trials before this technology should be approved and used in patients outside of carefully monitored studies.”