‘Averting’ contrast fails to limit AKI after coronary angiography
The Avert system successfully reduced contrast media volume but failed to trim the risk of acute kidney injury (AKI) following coronary angiography, according to a trial published in JACC: Cardiovascular Interventions.
Patients randomized to periprocedural hydration plus contrast injection with the contrast modulation system received 85.6 mL of contrast agent on average, compared to 101.3 mL among patients who were randomized to hydration alone. The reduction in contrast media volume (CMV) was largest when at least three vessels were treated via PCI—124 versus 232 mL, a 46 percent relative reduction.
However, the lower exposure to contrast agents didn’t translate to a significant difference in AKI; about 27 percent of people in both groups experienced contrast-induced AKI (CI-AKI), defined as an increase in serum creatinine of at least 0.3 mg/dL within five days of the procedure.
“Despite the absent effect on CI-AKI, CMV reduction is in general desirable and may be safely accomplished with the easy to use Avert system at low cost,” wrote lead author Roxana Mehran, MD, with Icahn School of Medicine at Mount Sinai in New York, and colleagues.
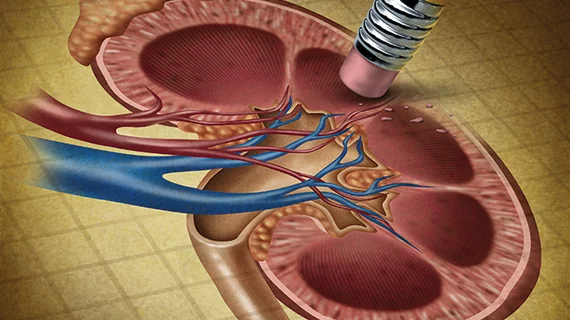
The Avert system, manufactured by Osprey Medical in Minnetonka, Minnesota, is designed to divert contrast agents during coronary injection. As the medium is manually injected into the patient, a portion of the fluid—determined by the injection force and the setting selected on the contrast modulator—is diverted into a reservoir. The rest is injected into the patient.
In this trial, 578 patients were enrolled after meeting criteria for a high risk of CI-AKI: baseline estimated glomerular filtration rate (eGFR) of 20-30 mL/min/1.73 m2 or eGFR between 30 and 60 mL/min/1.73 m2 along with two other risk factors.
Notably, the image quality was deemed acceptable in 99.3 percent of patients treated with the Avert system, despite the lower radiocontrast volumes.
“Because the amount of contrast diverted into the reservoir can be fine-tuned by adjusting the resistance of the reservoir line, in most cases the operator was able to compensate for any perceived deterioration in the degree of image opacification during the procedure,” the authors reported. “In addition, there were no significant differences in major adverse events between the two groups, with only one possible device-related event reported.”
Regarding the lack of difference in CI-AKI rates, the researchers pointed to the fact that two-thirds of study participants only underwent diagnostic angiography.
“Future trials designed specifically for a patient population requiring higher contrast volume, such as complex PCI, may be more reflective of potential risk reduction,” wrote Charles E. Chambers, MD, with Penn State Hershey Medical Center, in an accompanying editorial.
That being said, Chambers wasn’t entirely surprised at the high rates of AKI, even when contrast volume was reduced.
“End-stage renal disease is end stage; critically ill patients are critically ill,” he wrote. “No contrast dose is entirely safe in high-risk patients with other acute kidney injury etiologies, including dehydration, drug toxicities, hemodynamic instability, and atheroembolic or cholesterol-embolic disease.”
As investigators continue to search for the “holy grail” of CI-AKI prevention, Chambers suggested clinicians continue to focus on periprocedural hydration and contrast dose reduction to limit risk.