Cardiologists shed new light on treating severe tricuspid regurgitation in high-risk heart failure patients
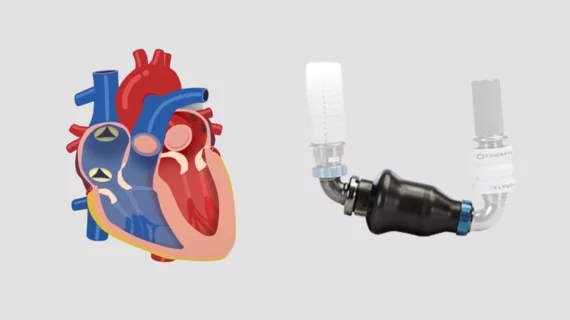
A team of interventional cardiologists has made a bit of history, using a new transcatheter device to treat tricuspid regurgitation (TR) in a high-risk heart failure patient who with a previously implanted left ventricular assist device (LVAD). It represents the first time this particular device, the TricValve Transcatheter Bicaval Valves System from P+F Products, has been implanted in a patient with this particular LVAD, the HeartMate II from Abbott.
The group detailed its experience in Circulation: Heart Failure.[1]
“Functional TR in the absence of leaflet abnormalities occurs frequently in heart failure patients due to annular dilatation,” wrote corresponding author Hiram Grando Bezerra, MD, an interventional cardiologist with the University of South Florida, and colleagues. “In the end-stage heart failure population with left LVADs, concomitant TR can be problematic and up to 25% of patients can have residual TR one year after LVAD implantation. This persistent TR contributes to morbidity and mortality, namely with right ventricular (RV) dysfunction.”
The 80-year-old female patient was experiencing persistent low-flow LVAD alarms in addition to other symptoms, including shortness of breath. She had already been hospitalized multiple times in the last year. She was initially viewed as a high-risk patient ineligible for surgical treatment, but was then approved for “compassionate use” of the TricValve device.
“Before the procedure, her volume status had attempted to be optimized as much as feasible without compromising LVAD flows, which was very challenging,” the authors added.
The device’s two valves were successfully implanted into the patient’s superior and inferior vena cava with assistance from fluoroscopy and a transesophageal echocardiogram. There were no complications, and the patient began experiencing immediate benefits. Nine months following the procedure, her TR “remained moderate” and she improved from New York Heart Association Class IV symptoms before the procedure to New York Heart Association Class I or II symptoms after the procedure. She also experienced a notable improvement in quality of life.
“It is believed that reducing her preload by addressing her TR subsequently reduced her peripheral congestion, which in turn improved her functional status,” the authors concluded.
The full study is available here.