Contrast injections during angiography, PCI unlikely to cause coronary injuries
Contrast media injections during percutaneous procedures are unlikely to cause or intensify coronary injuries beyond the very tip of the catheter, according to new data published in JSCAI.[1]
“There is a widely perceived idea that the hydraulic forces generated by contrast injections during angiography (pressure applied by hand or automated injectors) can either cause or propagate coronary dissections,” wrote first author Daniel Chamié, MD, PhD, an interventional cardiologist with Yale School of Medicine, and colleagues. “This mechanistic association between injection and injury is intuitively supported by the recognized risk of ventricular arrhythmias when coronary injections are performed into a small coronary branch (commonly the right-sided conus artery). Therefore, when a coronary dissection is suspected or confirmed, consensus-based practice recommends physicians limit the use of contrast injections to avoid worsening its severity and potentially putting the patient at risk of arterial occlusion or thrombosis.”
Do care teams really need to be limiting the use of contrast media due to these injection-related concerns? To learn more, Chamié et al. tracked coronary hemodynamics during contrast injections in 52 patients undergoing a clinically indicated coronary pressure wire assessment during coronary angiography or percutaneous coronary intervention (PCI). All patients were treated at one of four centers in Brazil, Mexico or the United Kingdom. Patients with vessels showing signs of severe coronary artery disease were excluded.
After administering ≥200 μg of nitroglycerine, researchers positioned a pressure sensor-tipped guidewire at five different predetermined locations to evaluate the impact of contrast injections. Recordings were taken at all locations that lasted a total of 60 seconds—these recordings included 10 seconds of resting recording, the contrast injection, contrast-induced hyperemia and then the recovery or resting conditions. While a majority of injections were manual, two of the participating facilities randomized between manual and automatic injections performed using an automatic injector pump. Pump settings were left up to the care teams.
Overall, 269 contrast injections were evaluated in 58 vessels. The mean patient age was 62.1 years old. The mean contrast volume dispensed per injection was 4.23 mL. Pump injections were associated with a higher mean volume (4.84 mL) than manual injections (3.79 mL). The left anterior descending artery was the target vessel in 56.9% of cases. The right coronary artery was the target of another 27.6% of cases, and the left circumflex artery made up the remaining 15.5%.
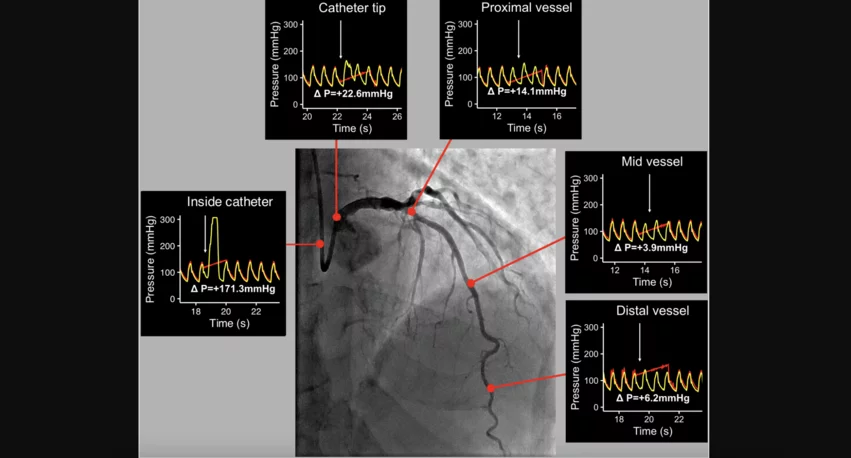
Chamié and colleagues did find that contrast injection was linked to a “small increase” in peak coronary pressures in the distal, mid and proximal segments of the coronary vessels. The mean peak pressure difference inside the catheter was 77.5 mm Hg. The mean peak pressure difference at the catheter’s tip, meanwhile, was 11.7 mm Hg.
Pressure changes were consistently higher closer to the guiding catheter tip, and they were the largest inside the catheter.
“Importantly, although beyond the catheter tip, the typical coronary waveform is not altered by contrast injection, it is completely lost inside the catheter with a sudden upright surge caused by injection forces,” the authors explained.
Performing injections manually or automatically did not appear to impact pressure changes in a significant way. On a similar note, the vessel being evaluated did not appear to make a significant difference.
Pressure changes suggest contrast injections not associated with significant risk
Reviewing their findings, the authors found little reason for alarm.
“Although statistically significant when compared to resting, the pressure changes observed during injections were very small in the proximal, mid and distal segments of all three vessels,” the group wrote. “Such values fall well within the known beat-to-beat variability of normal coronary pressures. Therefore, our data demonstrate that although some hydraulic force is needed to overcome the resistance imposed by the catheter, no residual force is significantly transmitted beyond the catheter tip, into the coronary artery itself.”
This suggests that intracoronary contrast injections could only potentially cause or propagate dissections close to the catheter, specifically if the catheter tip is inside the vessel at the time of the injection.
“Repeated and forceful injections should therefore be avoided when the area at risk is close to the catheter or when there are changes in aortic pressure waveform (pressure damping or ventricularization) suggesting catheter overengagement and/or ostial disease,” the authors added. “Dissections that occur beyond the proximal vessel segment, such as distal stent edge dissections or spontaneous coronary artery dissections (SCADs) should not be at risk of worsening with repeated injections, and consequently, contrast injection can be considered if clinically needed. The risk of propagating a dissection occurring beyond the proximal vessel segment during a SCAD assessment is more likely related to the advancement of wires and imaging catheters along the false lumen rather than to the injection of contrast media itself.”
Of course, vessel injuries can be caused by a variety of procedural factors; contrast injections are just one small piece of the puzzle.
A special note on contrast injections during CTO PCI procedures
Chamié et al. emphasized that special care should be taken when care teams are performing a chronic total occlusion (CTO) PCI.
“In CTO PCI, injection of contrast media into a closed extraluminal compartment is believed to increase the risk of extending a subintimal/intramural hematoma by exposing the false lumen to above-average pressures,” they wrote. “Although our data were not acquired during CTO procedures, our findings of extreme peak pressure changes inside the catheter support the recommendation of avoiding injections via antegrade catheters in such procedures. It is plausible that injection pressures could be transmitted to an enclosed extraluminal compartment, compressing the vessel lumen.
Final recommendations
Ultimately, the study’s authors concluded that care teams can feel comfortable and confident when performing contrast injections during coronary angiography and PCI.
“The hydraulic forces needed for contrast media injection during percutaneous procedures do not lead to a clinically significant increase in coronary pressures beyond the segments very close to the coronary catheter,” they wrote. “Although care should be taken during injections in cases of very proximal dissections or with catheter-induced pressure damping, it is unlikely that routine contrast injections would cause or worsen coronary injuries beyond the region close to the catheter.”
Click here to read the full analysis in JSCAI, the official journal of the Society for Cardiovascular Angiography and Interventions.