Intravascular imaging during PCI: Should cardiologists choose IVUS or OCT?
The use of intravascular imaging-guided percutaneous coronary intervention (PCI) has gained significant momentum in recent years. In fact, the American College of Cardiology issued a state-of-the-art review in 2023 that urged interventional cardiologists to guide PCI procedures with intravascular imaging whenever possible.
However, a key question remains: Out of the two most common intravascular imaging modalities, intravascular ultrasound (IVUS) and optical coherence tomography (OCT), is one a better overall choice than the other? A team of specialists explored that very topic, sharing their different thoughts on the two modalities in EuroIntervention.[1]
One perspective: IVUS linked to more value when guiding PCI procedures
“IVUS and OCT have distinct characteristics, such as penetration depth and axial resolution, that may make each of them more suitable for specific scenarios,” wrote first author Akiko Maehara, MD, an interventional cardiologist with the Columbia University Department of Medicine and Cardiovascular Research Foundation, and colleagues. “Current evidence on PCI guidance mainly consists of studies comparing intravascular imaging to angiography, with direct comparisons of IVUS and OCT with respect to clinical endpoints being quite limited.”
Maehara then listed some of the reasons care teams may want to side with IVUS over OCT. It is a better option for visualizing “the full thickness of the vessel wall” and determining the best device size for the job, for example. IVUS is also “technically easier to use” with no need for blood clearance. This makes IVUS the most effective modality for ostial lesions, left main coronary artery lesions and other complex patient cases.
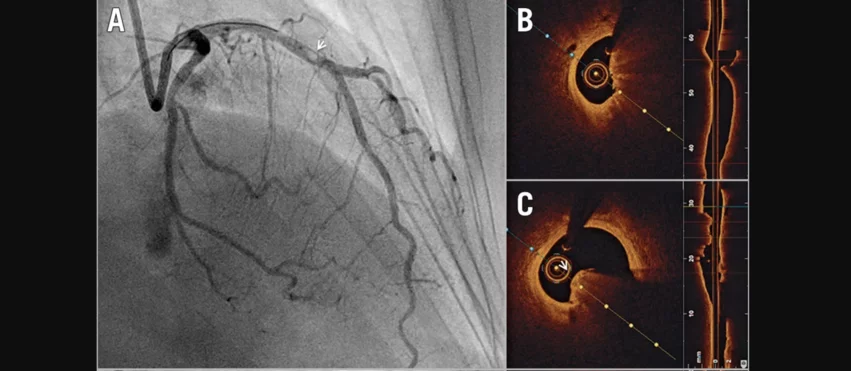
Optical coherence tomography-guided percutaneous coronary intervention on a calcific protruding nodule. A) Angiography shows a mid-left anterior descending (LAD) nodular obstruction (arrowhead). B) Optical coherence tomography (OCT) imaging reveals a small minimal lumen area and (C) confirms the aetiology of the obstruction to be a calcific protruding nodule (arrowhead). Images and caption courtesy of EuroIntervention and Ziad A. Ali, MD, DPhil, et al. DOI: 10.4244/EIJ-D-21-00089
In general, Maehara wrote, there is more evidence supporting the clinical value of IVUS-guided PCI than OCT-PCI. When exploring the history of randomized trials focused on this subject, it is easier to find studies that explored the potential benefits of IVUS than it is to find similar studies on OCT.
Another perspective: IVUS vs. OCT provide similar value
The EuroIntervention analysis then switched perspectives. Co-authors Jorge Sanz-Sánchez, MD, with La Fe University and Polytechnic Hospital in Valencia, Spain, and Hector M. Garcia-Garcia, MD, with MedStar Washington Hospital Center, explained why IVUS and OCT may actually be equals when it comes to guiding PCI.
“Direct comparisons in 3,324 patients show that there is no difference between OCT and IVUS for all clinical endpoints,” the authors wrote. “Further, a meta-analysis also showed that ‘indirect’ network comparisons are consistent with direct appraisals. Thus, at this point, one can conclude that IVUS does not have more robust data than OCT to inform PCI guidance.”
Those facts do not necessarily tell the full story. In recent years, researcher have identified different specific clinical scenarios where one modality may make more sense the other. Zero-contrast imaging-guided PCI “may be easier to set up using IVUS rather than OCT,” for instance.
Sanz-Sánchez and Garcia-Garcia emphasized that hybrid intravascular imaging systems make things much easier for cardiologists by offering both treatment options in the same catheter.
“As more hybrid systems become available, and providing they claim some of the market share, this comparison will no longer be necessary,” they wrote.
Concluding their thoughts on this topic, the authors noted that OCT and IVUS can both make a significant impact on patient care. Deciding which one to use should be based on the individual patient and not one rule that is permanently set in stone.
“Both modalities offer unique advantages and limitations, and their complementary use can enhance the safety and effectiveness of PCI,” they wrote.
Click here to read the full breakdown in EuroIntervention.
The three authors behind this evaluation did note that they have prior working relationships with many vendors in this space. Maehara has a history working with Boston Scientific, Abbott, Philips, SpectraWAVE and Nipro. Sanz-Sánchez, MD, has a prior history with Boston Scientific, Medtronic, Biosensors and Terumo. Garcia-Garcia, MD, has a history with Medtronic, Biotronik, Abbott, Neovasc, Corflow, Alucent Biomedical, Philips, Chiesi, Boston Scientific, Medis and ACIST.