IVL gains higher level of reimbursement with one of biggest coding updates for PCI in decades
Intravascular lithotripsy (IVL) therapy to break up calcified coronary lesions without vessel trauma from angioplasty using sonic waves will now be reimbursed at a higher rate under new in-hospital codes. These are the first new Medicare severity diagnosis related groups (MS-DRG) codes in 20 years for the percutaneous coronary intervention (PCI) space.
Shockwave Medical, the company that developed IVL technology, announced at the Transcatheter Cardiovascular Therapeutics (TCT) 2023 meeting that new, long-term reimbursement will be coming into effect in 2023 and early 2024. These will come in the form of coronary IVL-specific MS-DRG codes for hospital inpatient procedures. The bump in reimbursement is meant to cover more than the cost of the device and a physician current procedural terminology (CPT) Level I add-on code.
The new MS-DRG codes and payments became effective on Oct. 1, 2023.
The new reimbursement codes will provide a $8,000 increase on average nationwide for coronary IVL procedures compared to standard PCI DRGs. Shockwave said this is about a 55% increase in payment and more than covers the cost of the technology.
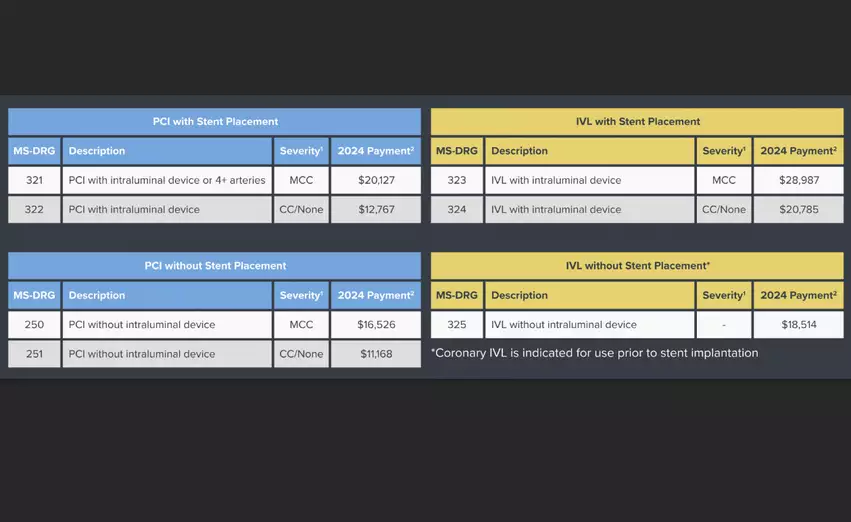
Shockwave said MS-DRG 323 for coronary IVL with an intraluminal device with major complications and comorbidities (MCC) the payment will be $28,987. MS-DRG 324 for coronary IVL with intraluminal device without MCC will be $20,785. MS-DRG 325 for coronary IVL without intraluminal device without MCC, the payment is $18,514.
For comparison, in-patient PCI plus a stent in a patient without co-morbidities it pays $12,767. With MCC, it goes up to $20,127.
"Combination therapy with multiple devices is necessary, but is also expensive. These changes in reimbursement means it is no longer going to be financially prohibitive to treat very complex patients who need multiple devices and the right tools. None of us ever want to make patient care decisions based on financial constrains. The changes that have taken place and that will take place on January 1, are going to make things a lot more simple and streamlined and make it easier to treat patients," explained Yousif Ahmad, MD, assistant professor of medicine and associate program director for interventional cardiology fellowship program at Yale, who has been involved with Shockwave and the reimbursement changes.
As proposed by the Centers for Medicare and Medicaid Services (CMS), the new CPT Level 1 add-on code provides physicians an additional 2.97 work relative value units (RVUs) for those employed by the hospital, and an estimated $140 payment for those in private practice. Shockwave said this is an increase of between 20-30% above the primary procedure regardless of what other technologies are used in the procedure in conjunction with coronary IVL, including atherectomy and percutaneous translumial coronary angioplasty (PTCA).
The bump in physician RVUs for performing coronary IVL is something interventional cardiologists have asked for since 2017.
Previously the payments for coronary IVL were through the Medicare Transitional Pass-Through Payment (TPT) program. The temporary reimbursement rate was approximately $3,000 per case.
TPT is designed to foster innovation and increase access to cutting-edge therapies that benefit patients. CMS said the program is important for hospitals to for products that offer substantial clinical improvement, but are not yet a standard of care with normal reimbursement channels.
Rise in IVL cases expected to follow higher reimbursement
Clinical trial data has shown the value of IVL to crack calcium without causing the vessel trauma common with non-compliant balloon angioplasty. However, many hospitals have been hesitant to invest in the technology. It is widely expected the new, higher payments will drive wider adoption of IVL.
A Shockwave spokesman said about 8% of PCI cases currently use IVL in the U.S., but all of these cases were at larger hospitals that were among the first adopters of the technology.
"With these changes, there is no longer the potential at the institutional level or the physician level for any financial penalty to using the device. That obstacle or hurdle is gone and we are now going to be liberated to just treat patients with the right tool at the right time and not have these constraints to worry about," Ahmad said.
Outpatient coronary IVL reimbursements
The TPT for coronary IVL procedures within the hospital outpatient setting will stay in place until mid-2024, when CMS will then determine which ambulatory payment classification (APC) coronary IVL will map to for long-term reimbursement.