Key interventional cardiology takeaways from ACC.22
Several late-breaking clinical trials at the American College of Cardiology (ACC) 2022 meeting will likely impact clinical practice. Below are summaries of a few key trials and their takeaways for interventional cardiology and structural heart interventions.
TAVR valve deterioration lower that surgical valves
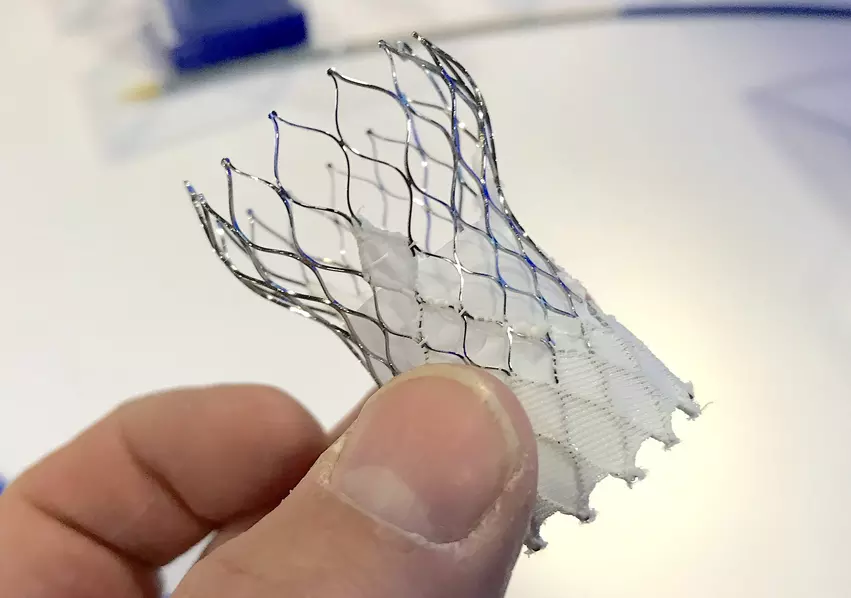
A long standing question has been the durability of transcatheter aortic valve replacement (TAVR) systems compared to traditional surgical aortic valve replacement (SAVR) devices. It has always been assumed SAVR would out-perform TAVR, but new data from a late-breaking review of the CoreValve U.S. pivotal and SURTAVI trials showed this was not the case, making it one of the key take-away trials presented at ACC this year.
Patients who received a transcatheter supra-annular, self-expanding, CoreValve had significantly less structural valve deterioration (SVD) after five years compared with similar patients who had the biologic SAVR valve. TAVR is now approved by the U.S. Food and Drug Administration (FDA) for use in patients of all ages and risk levels who need a replacement heart valve. But, heart teams often refer younger patients for surgery because of increased durability.
"For moderate and greater regurgitation patients, TAVR did better than surgery," said Michael J. Reardon, MD, professor of cardiothoracic surgery and Allison Family Distinguished chair of cardiovascular research at Houston Methodist DeBakey Heart and Vascular Center and the study’s senior author. "We know these TAVR valves have superior hemodynamics compared to surgical valves in every randomized trial and timepoint we tested. And this might be why surgery is behind the 8-ball when it begins, and why TAVR has a head start."
SVD is only an issue with bioprosthetic valves and is the most frequent cause of valve failure. SVD includes problems such as scarring, thickening/calcification of the leaflets hardening, and fracturing of the valve frame.
Reardon said 10-year data on the intermediate and low risk trials is being collected to determine the valve deterioration level in these patients using TAVR and SAVR. "We will get 10 year data in a lower risk, younger group of patients that are going to live longer and we are going to find out which valves last longer," he said.
There is still a lot of apprehension on heart teams about sending younger patients, since they will likely live much longer than elderly patients who are more of the typical candidates for TAVR. The metal support frame used in TAVR valves gets embedded in the wall of the heart and can complicate later open heart surgical valve replacement procedures. However, if TAVR valves show they can last longer than surgical valves in most patients, there will likely be a shift toward a younger TAVR population.
“Heart surgeons tend to worry that in younger, lower-risk patients, replacement valves inserted using TAVR may fail more quickly than surgically inserted valves,” Reardon said. “The results of this study suggest exactly the opposite — that at five years, the TAVR-inserted valve has less structural deterioration than the surgically inserted one.”
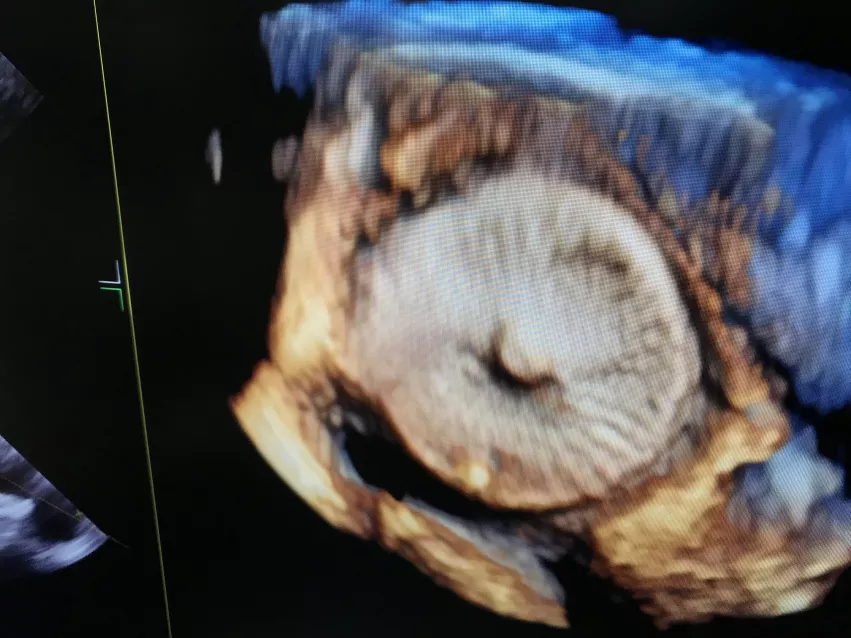
NCDR LAAO Registry: Clinical impact of residual leaks following LAA occlusion
This analysis of the National Cardiovascular Data Registry (NCDR) Left Atrial Appendage Occlusion (LAAO) Registry was the first study to show that peri-device leak is associated with increased stroke risk. The ACC late-breaking data showed peri-device leak is associated with increased stroke risk, so LAAO operators should assess devices carefully for leak and strive to leave no leak, explained Andrew M. Goldsweig, MD, MSc, RPVI, FSCAI, associate cath lab director for structural heart disease, University of Nebraska Medical Center and associate editor for the Journal of the Society of Cardiovascular Angiography and Interventions (SCAI).
The study examined rates of a primary endpoint composite of stroke, transient ischemic attack, and systemic embolism among LAAO patients stratified by no leak, small leak (less than 5 mm), and large leak (more than 5 mm). Among 51,333 patients undergoing LAAO with the Watchman 2.5 device (Boston Scientific, Marlborough, MA) from 2016 through 2019, 37,696 (73.4%) had no leak, 13,258 (25.8%) had small leaks (<5 mm), and 379 (0.7%) had large leaks (>5 mm). The presence of a small leak was associated with a slightly higher rate of the primary endpoint (adjusted HR 1.152, 95% confidence interval [CI] 1.025-1.294), major bleeding (HR 1.11, 95% CI 1.029-1.120), and any major adverse events (HR 1.102, 95% CI 1.048-1.160).
Large leaks were not statistically associated with adverse events, although more patients with large leaks continued anticoagulation.
The NCDR LAAO Registry is the largest LAAO dataset in the world, including every commercial LAAO procedure performed in the U.S. However, Goldsweig said the study was subject to the usual cadre of biases inherent when performing a retrospective analysis of a large data registry, particularly information bias.
Tricuspid valve repair with the Edwards Pascal transcatheter clip at 1 year — CLASP TR
Severe symptomatic tricuspid regurgitation (TR) is prevalent and causes significant morbidity. This prospective, single-arm multicenter early feasibility study was designed to evaluate the safety and performance of the Pascal transcatheter valve repair clip system in symptomatic severe TR. The device is similar to the functionality of the MitraClip, in that its arms clasp the leaflets to the valve to perform a transcatheter edge-to-edge repair (TEER).
Surgical intervention is not commonly utilized in TR, compared to left sided valve disease and there are questions regarding outcomes with surgical intervention in advanced stages, explained Kalkidan Bishu, MD, MS, FSCAI, an interventional cardiologist at Essential Health St. Mary’s-Heart and Vascular Center, and an SCAI Council member. He said there is a need for, and a lot of interest in, a percutaneous intervention for native valve TR.
The study included 65 patients (mean age 77; 55% women) with severe symptomatic TR despite medical therapy underwent treatment using Ewards Pascal Transcatheter Repair System. Primary endpoint was the composite of major adverse events at 30 days with follow up at six months and then annually. One-year follow up results were reported for 46 out of 65 patients in whom follow-up data was available (loss of follow up attributed to COVID-19 pandemic). Mortality was 10.8%. About 18 % were hospitalized for heart failure and 16.9% experienced a major adverse event, the most common adverse event was bleeding at 9.2%. The majority of patients improved. Heart failure severity, six-minute walk test and quality of life were improved.
"Tricuspid valve regurgitation is a big and growing problem for us, and there is about a 30% mortality rate," said Adam Greenbaum, MD, co-director, Structural Heart and Valve Center, Emory University, who presented the study at ACC. "We don't have good therapies to offer these patients other than diuretics, and surgery is associated with high rates of morbidity and mortality because the patients are so sick, frail and elderly.
However, he said this opens the door for minimally invasive procedures such as the Pascal and MitraClip in these patients. "We were able to achieve a reduction of 86% in TR, reducing it to moderate for less, and most patients had a two grade reduction," Greenbaum said.
Trends and final results of the North American COVID-19 Myocardial Infarction (NACMI) Registry
NACMI was established in 2020 to characterize the presentation profiles, treatment and outcomes for patients who were hospitalized with ST-elevated myocardial infarction (STEMI) in the context of confirmed COVID-19 infection. A significant drop in in-hospital mortality was observed in the 2021 cohort as compared with the 2020 cohort. The investigators also found a significant drop in the secondary composite endpoint of death, stroke, or a repeat myocardial infarction from 35% in 2020 to 25% in 2021. Reductions were largely associated COVID vaccinations.
In 2020, it quickly became apparent that COVID-19 infection also encompasses a variety of cardiac and vascular manifestations, including hypercoagulability with extensive formation of venous and arterial thrombus, acute coronary syndromes (ACS), elevated risk for STEMI and sudden cardiac death. The risk for STEMI is now known to persist for several weeks after the onset of clinical COVID-19 infection, explained Sandeep Nathan, MD, MSc, FSCAI, co-director, cardiac cath lab, University of Chicago. He NACMI was created as a collaboration between the SCAI, the ACC Interventional Council, and the Canadian Association of Interventional Cardiology (CAIC).
The NACMI Investigators analyzed data from 586 patients: n=227 in the 2020 cohort and n=359 in the 2021 cohort.
In April 2021, Garcia et al. reported that the primary endpoint of in-hospital mortality for COVID-19 infection complicated by STEMI was 33% (75/227) in 2020, a figure which dropped to 23% (83/359) in 2021.
The notable reduction in COVID-19 STEMI mortality was likely related to the lower incidence of cardiogenic shock and concomitant pulmonary manifestations in 2021, both of which significantly increased mortality when present.
Vaccination data was available for 54% (193/359) of the 2021 cohort and found that 0% of vaccinated patients suffered in-hospital mortality while 22% of unvaccinated patients died in 2021, a value which is significantly higher than historical (pre-COVID-19) estimates of in-hospital STEMI mortality.
There was a significant drop in in-hospital mortality (the primary endpoint) observed in the 2021 cohort as compared with the 2020 cohort.
The investigators also found a significant drop in the secondary composite endpoint of death, stroke, or a repeat myocardial infarction from 35% in 2020 to 25% in 2021.
Learn more about this study in the VIDEO: Vaccines boosted survival among STEMI patients with COVID-19 — Interview with Santiago Garcia, MD, who presented the data.
FAME 3 Quality of life after FFR-guided stunting vs. coronary bypass
This study compared multi-vessel coronary artery disease treated with coronary artery bypass graft (CABG) to fractional flow reserve (FFR)-guided percutaneous coronary intervention (PCI). The data show these have similar quality of life, angina relief and return to work outcomes. But, FFR-guided PCI resulted in a faster improvement in quality of life than CABG during the first year after revascularization, and improved working status in patients younger than 65 years old, explained Luai Tabaza, MD, an interventional cardiologist at Virtua Health in Philadelphia, which summarizing the study for SCAI members.
This quality-of-life sub study showed that FFR-guided PCI have similar quality of life and angina relief compared to CABG at one year, in the younger than 65 year-old group, CABG was associated with less return to work compared to PCI at 1, 6 and 12 months, Tabaza said.
Management of patients with multi-vessel coronary disease is a clinical challenge we face every day, FAME-3 compares the two main treatment options, FFR-guided PCI and CABG," Tabaza said.
The primary end point was major adverse cardiac and cerebral events (MACCE) and repeat revascularization, PCI did not meet non-inferiority at one year as presented at TCT in November 2021. Both study arms had low event rates, and the differences between PCI and CABG narrowed compared to previous studies, which prompted the quality-of-life sub-study to further aid in clinical decision making.
Comparison of FFR-guided and IVUS-guided PCI in intermediate coronary artery stenosis — FLAVOUR randomized trial
This clinical trial offers the first head-to-head comparison of FFR guided vs. intravascular ultrasound (IVUS)-guided PCI for intermediate coronary lesions. The study showed both are an appropriate initial strategy for intermediate lesions and results in reduced resource utilization for coronary stenting.
FFR is an appropriate initial strategy to evaluate intermediate stenosis , which makes up between 40-70% lesions. When FFR was compared to IVUS, there were fewer stents placed (44.5 vs. 65.3%), summarized Tanveer Rab, MD, FSCAI, a professor and an interventional cardiologist at Emory University, and an SCAI committee member. He said there were no statistically significant differences in the rates of death, myocardial infarction or repeat revascularization in either the FFR or IVUS group (8.1 vs. 8.5% (p< 0.001 for non-inferiority).
COMPLETE Trial: Effects of complete revascularization on angina-related quality of life in STEMI patients
This sub-study questioned whether the complete revascularization strategy for early PCI for STEMI would improve the patient's overall quality of life and whether this improvement was durable over a 3-year follow-up. The results of the study revealed that the completely vascular strategy improved the PCI self-assessment questionnaire (SAQ) overall score, quality of life score treatment satisfaction score, physical limitations score and angina frequency score.
This study presented at ACC22 is a sub-study of the complete trial which was published in 2019, explained Gary S. Ledley, MD, FSCAI, a, interventional cardiologist at Tower Health, in Phoenixville, Pa. The prospective randomized trial looked at complete versus culprit-only revascularization to treat multivessel disease after early PCI for STEMI. In this trial approximately 2,000 patients were randomized to each arm. There were followed for three years. The overall results confirmed that the strategy of complete revascularization post STEMI reduced the endpoints of death or myocardial infarction (MI) and the combination endpoint of death MI or ischemia directed revascularization.
The results of the study revealed that the completely vascular strategy improved the SAQ's overall score, quality of life score treatment satisfaction score, physical limitations score and angina frequency score. In addition, both the complete revascularization and the culprit lesion only, strategy resulted in substantial improvement in overall angina related quality of life compared with baseline. At a median of 3-year follow-up a greater proportion of patients were free of angina in the complete revascularization group than in the culprit lesion only group, translating into a number needed to treat of 31 patients to prevent one patient from experiencing angina and a median follow-up of 3 years.
Ledley said physicians can provide this information to patients in the context of shared decision-making as it relates to coronary artery vascularization patients with STEMI.