Novel device treats pulmonary embolism without clot-dissolving drugs
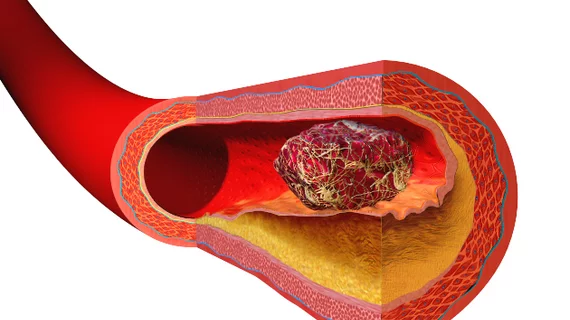
A new device allows clinicians to remove blood clots from the pulmonary arteries and improve right ventricular function without the use of thrombolytics, according to a late-breaking clinical study presented April 26 at SCAI 2018 in San Diego.
The single-arm multicenter trial evaluated outcomes of 106 patients treated with the FlowTriever system (Inari Medical, Irvine, California) in the setting of pulmonary embolism. The patients saw a drop in their right ventricular to left ventricular (RV/LV) ratios from 1.53 at baseline to 1.15 two days after clot removal.
The FlowTriever device is placed in a large-bore catheter and navigated to the site of the clot, where it is deployed to remove the thrombus. Procedures took an average of 94 minutes in the study.
Sixty-seven patients (63 percent) required one day or less in the intensive care unit (ICU), while one-fifth needed at least three days. The mean ICU stay was 1.5 days post-procedure. One patient died and four experienced major adverse events including cardiogenic shock, worsening pulmonary embolism, pulmonary infarction and respiratory arrest.
“The outcomes that we saw in this trial are extremely favorable because the improvement in the size and function of the right ventricle was comparable to previous results we’ve seen with thrombolytic therapy,” coauthor Thomas Tu, MD, with Baptist Health Louisville, said in a press release. “Our study paves the way for this novel treatment option for patients with pulmonary embolism and shows that we can decrease their risk of bleeding complications while potentially being just as safe and effective.”
Tu and colleagues said the next step is evaluating the FlowTriever against standard therapy in a randomized study.