CMS changes coverage policy for carotid stenting to make it more widely available
A group of interventional cardiology and vascular surgery experts has successfully petitioned the Centers for Medicare and Medicaid Services (CMS) to change its national coverage determination (NCD) for carotid artery stenting (CAS) procedures. This will make it much easier for more patients to receive the minimally invasive procedure as an alternative to open surgical carotid endarterectomy (CEA). Providing CAS reimbursement for a wider patient population is also expected to expand its use.
Clinical trials over the past decade have showed minimally invasive CAS was about equal in outcomes to open surgical CEA. However, restrictions on carotid stenting reimbursements have largely limited its use. As of Oct. 11, this is no longer the case, thanks to the Multispecialty Carotid Alliance (MSCA), a group of key opinion leaders in interventional cardiology, neurology and vascular surgery. The group sent a formal request in June 2022 for CMS to review its policy based on the new clinical data, which resulted in the policy changes last week.
MSCA applauded the CMS policy change in a statement this week. The group said the decision will ensure Medicare patients will have access to the full range of therapies that are available. This includes carotid endarterectomy (CEA), transfemoral carotid artery stenting (TF-CAS), transradial carotid artery stenting (TR-CAS), and transcarotid artery revascularization (TCAR). The MSCA also emphasized that optimal medical therapy (OMT) remains the foundation for treatment, and CAS, CEA or TCAR should be offered only to those who are deemed appropriate for revascularization on top of OMT.
"We believe that their thorough analysis and the challenging deliberations that they undertook ultimately led to a decision that is in the best interest of Medicare beneficiaries and the American public," MSCA said in its statement.
"The Carotid NCD is great news for patients. Medicare patients, and presumably patients covered by other payers, will now have access to the full range of revascularization options for reduction in stroke risk, including CAS, TCAR, and CEA. Interestingly, in their decision, the Coverage Analysis Group (CAG) of CMS basically said that stenting is a good therapy for carotid stenosis, regardless of how that stent is delivered, whether by femoral, radial, or trans-carotid approach. CMS also emphasized that use of CAS CEA should be reserved for only those carefully selected patients in whom revascularization on top of optimal medical therapy is deemed appropriate," said Ken Rosenfield, MD, section head of vascular medicine and intervention, and chairman of STEMI and Acute MI Quality Improvement Committee at Massachusetts General Hospital, and one of the leaders of the MSCA effort.
The MSCA is now urges all stakeholders to join forces to ensure safe and proper implementation of this decision so that patients receive the highest quality and most appropriate care. The MSCA says its experts involved in neurology, vascular surgery and interventional cardiology are is ready to work with CMS, medical societies and other professional medical organizations, industry partners, and patient representatives to achieve this goal.
The Society for Cardiovascular Angiography and Interventions (SCAI) strongly supported the push to make this update.
"We have worked for the better part of 20 years to demonstrate the safety and efficacy of CAS as compared to carotid endarterectomy and medical therapies alone by producing high quality clinical evidence. Our multi-disciplinary approach now provides physicians and patients increased access to this safe and minimally invasive therapy for treatment of carotid artery disease alongside other excellent options including carotid endarterectomy and TCAR so that patients and physicians can collectively make the best decision for themselves,” Adnan Siddiqui, MD, a professor and vice chairman in the department of neurosurgery at the State University of Buffalo, said in a statement from carotid stent vendor Cordis. Siddiqui was one of the physicians involved in the MSCA effort to change the CMS overage determination.
Cordis said CAS has been demonstrated to be a safe and efficacious therapy, with over 35,000 procedures performed annually.
While the NCD changes were supported by numerous cardiology and neurology medical societies, it was opposed by one, the Society for Vascular Surgery (SVS). Interventional stenting procedures have been seen as competition to the tranditional standrad of care with vascular surgery. It echos the similar to the competition between cardiac surgeons and interventional cardiology 20 years ago. Cardiac surgeons also opposed widening use of coronary stent procedures in the 1990s and 2000s.
"We believe the coverage expansion outlined in the updated NCD 20.7 is premature given the pending results of the National Institutes of Health-funded CREST 2 (The Carotid Revascularization and Medical Management for Asymptomatic Carotid Stenosis Study) Trial and holds significant potential to increase risk in achieving quality of care and patient safety, particularly for our most vulnerable elderly patients," SVS said in a statement opposing the policy change this week.
What is different about the new CMS coverage determination for carotid stenting?
The old CMS coverage determination stated CMS would only pay for CAS procedures in patients who are at high risk for CEA and who also have symptomatic carotid artery stenosis of 70% or more. The decision on who is a poor surgical candidate also needed to be made by a surgeon.
The new policy states carotid stenting with embolic protection devices is now covered for patients with symptomatic carotid artery stenosis of 50% or more, or asymptomatic carotid artery stenosis 70% or more occlusion. The determination for need is also now changed to a shared decision making process with a neurologist using imaging with proven clinical value from trials.
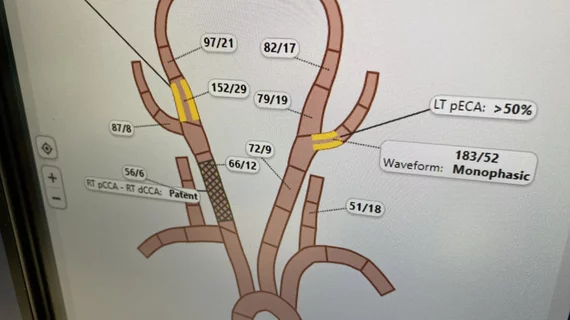
Neurological assessment by a neurologist or NIH stroke scale (NIHSS) certified health professional before and after CAS must be performed. CMS said the first-line evaluation of carotid artery stenosis must use duplex ultrasound. Computed Tomography (CT) angiography or magnetic resonance imaging (MRI) angiography, if not contraindicated, must be used to confirm the degree of stenosis and provide additional information about the aortic arch, and extra- and intracranial circulation.
CMS said intra-arterial digital subtraction angiography may be used only when there is significant discrepancy between noninvasive imaging results, or in lieu of CT angiography or MRI angiography if these are contraindicated.
Prior to performing a CAS procedure, CMS also said the practitioner must engage in a formal shared decision-making interaction with the beneficiary. The shared decision-making interaction must include:
• Discussion of all treatment options including CEA, CAS (which includes TCAR), and OMT.
• Explanation of risks and benefits for each option specific to the beneficiary’s clinical situation.
• Integration of clinical guidelines (e.g., patient comorbidities and concomitant treatments).
• Discussion and incorporation of beneficiary’s personal preferences and priorities in choosing a treatment plan.
Hospitals performing carotid stenting no longer need to be certified
The old CMS coverage determination policy required a facility to be certified to perform CAS, which is eliminated in the new coverage determination. CMS said this NCD does not require approval or a third-party facility approval, accreditation or certification for coverage purposes.
CMS did state that facilities performing CAS must establish and maintain institutional and physician standards to support a dedicated carotid stent program. These standards must at least include and ensure the following:
• Facilities have a clearly delineated program for granting carotid stent privileges and for monitoring patient outcomes for individual physicians and the program as a whole.
• The oversight committee for this program shall be empowered to identify the minimum case volume for a physician to maintain privileges, as well as the (risk-adjusted) threshold for complications that the institution will allow before suspending privileges or instituting measures for remediation. Committees are encouraged to apply published standards from specialty societies and widely-used, published professional society guidelines to determine appropriate physician qualifications.
• Facilities have appropriately trained staff capable of fulfilling roles and responsibilities as delineated under the dedicated carotid stent program.
• Facilities have appropriate supporting personnel and equipment for imaging, emergency management, advanced physiologic monitoring, and other ancillary care.
• Facilities must ensure continuous quality improvement by assessing procedural outcomes and making necessary programmatic adjustments to ensure patient safety.
In addition to the national coverage described above, CMS said Medicare administrative contractors (MACs) may make reasonable and necessary determinations under section 1862(a)(1)(A) for any other beneficiary seeking coverage for PTA of the carotid artery concurrent with stenting.
History of Medicare coverage for carotid stenting
Medicare began covering CAS nationally in March 2005, when CMS implemented coverage with specific criteria for patient selection, facility requirements and operator qualifications. The policy was last reviewed in 2009.
MSCA called for reconsideration of the CMS NCD for CAS in 2022 because there has been an extensive amount of new clinical evidence generated over the past 13 years. MSCA said these studies demonstrate CAS improves health outcomes in broader patient populations than currently covered by CMS.
Stroke therapy is evolving
Like atherosclerotic cardiovascular disease that can lead to coronary artery occlusion causing ischemia and heart attacks, stroke is caused by a similar atherosclerotic disease process in the carotid arteries. Cardiology has advanced frontline treatments for ischemia and heart attacks using minimally invasive percutaneous coronary intervention (PCI) with balloon angiography and stents. However, similar therapy for stroke is still mostly open carotid surgical procedures or the use of TpA during acute strokes, similar to how heart attacks were treated 30 years ago.
Interventional treatments for stroke are on the rise and becoming a standard of care at most large stroke centers. Similar to a cardiac cath lab working to activate early to receive an incoming ST-elevated myocardial infarction (STEMI) patient quickly so they can meet the recommended door-to-balloon time of 90 minutes or less, many stroke centers are now using a similar early activation to quickly revascularize arteries in the brain.
Interventional cardiology has become increasing involved in this space at some centers as treatments move more toward minimally invasive percutaneous approaches.