New AFib guidelines include higher recommendations for catheter ablation, LAAO
The American College of Cardiology (ACC) and American Heart Association (AHA) have published new guidelines for the diagnosis and management of atrial fibrillation (AFib). Cardiologists, electrophysiologists, surgeons, pharmacists, patient representatives and other stakeholders all collaborated on the updated recommendations.
The document, available in both the Journal of the American College of Cardiology and Circulation, includes several key updates compared to previous industry guidelines.[1, 2] For instance, it embraces more aggressive treatments such as catheter ablation and left atrial appendage occlusion (LAAO) due to the latest clinical data.
“The new guideline reinforces the urgent need to approach AFib as a complex cardiovascular condition that requires disease prevention, risk factor modification, as well as optimizing therapies and patients' access to care and ongoing, long-term management,” cardiologist Jose Joglar, MD, head of the arrhythmia program at UT Southwestern Medical Center and chair of the document’s writing committee, said in a statement. “This is a complex disease. It's not just an isolated disorder of the heart's rhythm, and we now know that the longer someone is in AFib, the harder it is to get them back to normal sinus rhythm.”
Key takeaways from the 2023 ACC/AHA/ACCP/HRS AFib guidelines
1. Lifestyle changes/risk factor modifications must be communicated to patients. One important difference compared to previous guidelines is how detailed the writing committee was when describing the different ways a patient can improve their health through everyday changes in their day-to-day life.
“Many patients don’t know where to start when they are given advice about lifestyle modification, so we are very specific with our recommendations,” Joglar explained. “For example, instead of saying ‘you need to exercise,’ which is largely unhelpful to patients, we recommend talking with patients about what types of physical activity works for them and how many minutes they should be active each day or each week.”
2. Catheter ablation is safe, effective and can be used as a first-line option for some patients. Catheter ablation technology has rapidly evolved in recent years, and the industry has clearly been paying attention. The minimally invasive treatments, which involve targeting specific cardiac tissues to improve a patient’s heart rhythm, received a Class 1 treatment recommendation for certain patient, including those who present with both AFib and heart failure with reduced ejection fraction (HFrEF). While catheter ablation was previously seen as a second treatment option once other techniques were unsuccessfully, the writing committee has now acknowledged that certain patients may receive the best possible care if they are treated with catheter ablation right away.
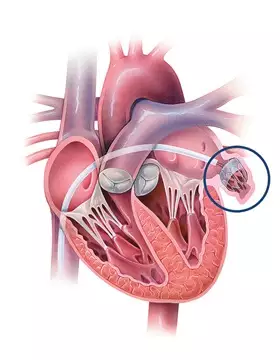
3. LAAO devices can deliver significant value. Surgically closing the left atrial appendage (LAA) can greatly reduce the risk of stroke among patients with nonvalvular AFib, though cardiologists typically begin with oral anticoagulants (OACs). In patients where OAC use is not recommended, or simply not effective, LAAO provides an alternative way to limit the risk of thromboembolism in the LAA.
In these updated guidelines, LAAO receives higher recommendations than ever before. It is seen as a “reasonable” among patients with a “CHA2DS2-VASc score ≥2 and a contraindication to long-term OAC” and a “reasonable alternative” among “patients with a moderate to high risk of stroke and a high risk of major bleeding on OAC.”
4. Flexibility when using clinical risk scores is important. While the CHA2DS2-VASc score is an essential resource for knowing when a patient’s stroke risk is elevated, the writing committee noted that other tools are also available to clinicians.
“Patients at an intermediate annual risk score who remain uncertain about the benefit of anticoagulation can benefit from consideration of other risk variables to help inform the decision, or the use of other clinical risk scores to improve prediction, facilitate shared decision making, and incorporate into the electronic medical record,” the group wrote.
Additional information about the updated AFib recommendations
The American College of Clinical Pharmacy (ACCP) and Heart Rhythm Society (HRS) have fully endorsed these new guidelines, and the writing group included representatives from both groups.
The full ACC/AHA/ACCP/HRS guidelines can be read here and here.