Real-world Watchman patients experiencing fewer complications after LAAO than seen in clinical trials
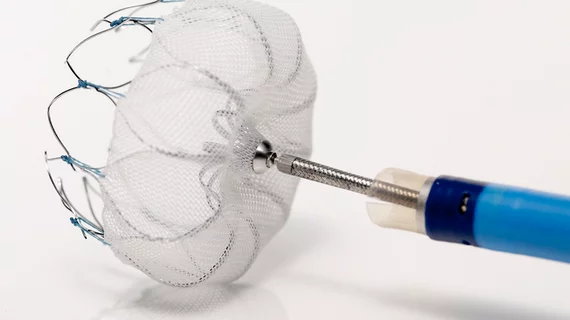
Atrial fibrillation patients who underwent left atrial appendage occlusion (LAAO) with the Watchman device after it gained U.S. FDA approval have experienced fewer complications and faced a lower risk of ischemic stroke than patients included in the PROTECT-AF and PREVAIL clinical trials, according to new findings published in JACC: Cardiovascular Interventions.[1]
“The rapid adoption of Watchman LAAO by an increasing number of operators in populations that are likely to carry a significant burden of coexisting illnesses requires scrutiny, particularly considering the periprocedural risks observed in the clinical trials,” wrote first author Daniel J. Friedman, MD, a cardiovascular specialist from the department of internal medicine at Yale University School of Medicine, and colleagues.
Friedman et al. noted that Watchman operators are required to report LAAO procedures to a national registry — the NCDR LAAO Registry — to receive payment, making the registry a “nationally representative repository for data on commercial Watchman implantation in the United States.” To gain a better understanding of patient outcomes associated with the Watchman device, the group matched 1,904 registry patients to 667 LAAO patients.
Overall, pericardial effusion requiring intervention (3.8% vs. 0.6%), periprocedural ischemic stroke (0.9% vs. 0.2%) and failed device implantation (7.5% vs. 3.6%) were all more common during the PROTECT-AF and PREVAIL clinical trials than among patients in a real-world setting.
“Rates of periprocedural complications with LAAO in the pivotal clinical trials generated concerns regarding whether procedural risks would overwhelm any longer-term benefit,” the authors wrote. “Pericardial effusion requiring drainage and ischemic stroke in the context of device implant failure rates of 12% in PROTECT-AF and 5% in PREVAIL likely contributed to the delay in FDA approval. Notably, changes in technique allowing for safer access of the left atrial appendage and device deployment lowered the risk of pericardial effusion throughout the course of the trials, and rates of mild stroke, likely related to air emboli, also decreased. The current study demonstrates that in matched patients from the NCDR Registry, the rate of pericardial effusion requiring intervention and ischemic stroke have continued to decline, whereas the rate of successful implantation has increased.”
Zooming out a bit, the authors also found that LAAO patients treated in a real-world setting faced a lower 425-day risk of ischemic stroke than those treated during the PROTECT-AF and PREVAIL trials (2.7% vs. 1.21%). While the 425-day risk of hemorrhagic stroke was comparable between the two groups, the risk of patient mortality after 425 days was actually higher among patients treated in a real-world setting (6.23% vs. 2.92%). This different, the authors noted, is “attributable to noncardiovascular deaths.”
“These results suggest improving safety and efficacy of Watchman LAAO in clinical practice and highlight the value of a national registry in understanding the adoption of technology and assessing procedural outcomes in contemporary practice,” the authors concluded.
Related Structural Heart Disease Content:
Same-day discharge after LAAO associated with strong outcomes, significant cost savings
Interventional cardiologists complete first heart procedure of its kind in North America
TAVR outcomes unaffected when women require a smaller valve prosthesis
Reference: