Boston Scientific TAVR valve linked to positive outcomes after next-day discharge
Next-day discharge (NDD) after transcatheter aortic valve replacement (TAVR) with Boston Scientific’s line of self-expanding heart valves is safe and feasible, according to new data published in the American Journal of Cardiology.[1]
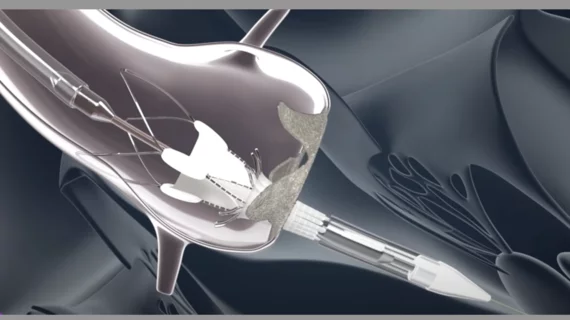
The Acurate neo and neo2 aortic valve systems have both received CE mark approval. In the United States, however, they are not yet approved by the U.S. Food and Drug Administration.
“A major step forward in the management of patients undergoing TAVR has been the establishment of institutional pathways for early discharge,” wrote corresponding author Rodrigo Bagur, MD, PhD, with the London Health Sciences Center in Ontario, Canada, and colleagues. “However, these early discharge protocols were for selected patients and using selected transcatheter heart valves.”
According to Bagur et al., Boston Scientific’s transcatheter heart valves have been underrepresented in previous research exploring the effectiveness of NDD. They hoped to reverse that trend, exploring data from more than 350 patients treated at a single London, Canada, facility from 2018 to April 2023. All patients underwent transfemoral TAVR with the Acurate neo or neo2 aortic transcatheter heart valve. The mean age was 84 years old, and 61% of patients were women.
Overall, 55.4% of patients followed a NDD pathway. Another 18.8% of patients were discharged between 24 and 48 hours after TAVR, and the remaining 25.8% were discharged at least 48 hours after TAVR. Patients in the NDD group had lower mean Society of Thoracic Surgeons Predicted Risk of Mortality (STS-PROM) scores prior to treatment than patients discharged after 24-48 hours. As one may expect, patients discharged at least 48 hours after TAVR had higher STS-PROM scores than the other two groups.
“As expected, individuals who had procedural-related complications were more often discharged more than 48 hours, but no difference was encountered between the NDD and 24-48 hour groups,” the authors wrote.
New permanent pacemaker implantation (PPI) was seen in 2.2% of NDD patients, 8.6% of 24-48 hour patients and 24% of more than 48 hour patients. Five strokes were seen, all in more than 48 hour patients. There were “no significant difference” between the three groups in terms of vascular complications, bleeding events or infections.
Once patients were sent home, there were no deaths after 30 days. The primary outcome—all-cause readmissions soon after discharge—was not statistically different between the three groups. However, readmissions at the 30-day mark were much more common among patients discharged at least 48 hours after treatment.
“Despite an all-comer population with a mean age of 84 years old, we had 0% mortality after hospital discharge through 30 days, and the overall all-cause readmission rate at 30 days was 9.3% following an NDD pathway,” the group concluded. “Sixty percent of the readmissions were for cardiovascular causes, which were evenly distributed among those presenting with conduction disturbances requiring PPI and congestive heart failure. The present study also shows the absence of significant differences in overall all-cause unplanned readmissions across the groups. However, those who were discharged after more than 48 hours experienced almost twice as high the proportion of readmissions at 30 days, highlighting, therefore, the safety of NDD and early discharge at 24-48 hours.”
Boston Scientific did not fund or support this analysis in any way. Click here for the full study.