Cerebral protection during TAVR linked to lower risk of major stroke, other key benefits
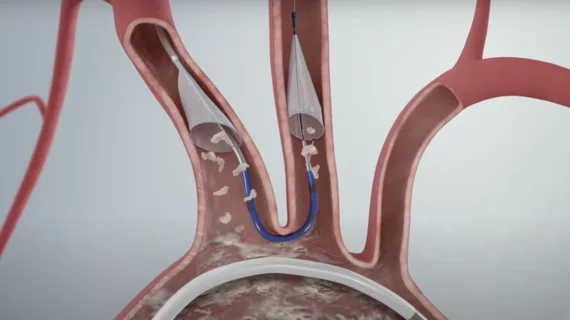
Strokes remain one of the most substantial side effects of transcatheter aortic valve replacement (TAVR), occurring in approximately 2% of patients following treatment. Cerebral protection devices (CPDs) such as the Sentinel Cerebral Protection System from Boston Scientific are designed to help alleviate this issue. They work by capturing and removing loose debris before it reaches the brain, but early studies have not identified a significant shift in stroke rates.
To learn more about how CPDs may impact TAVR outcomes, a team of researchers with Cleveland Clinic’s Heart Vascular and Thoracic Institute tracked data from more than 270,000 patients. The group shared its analysis in the Journal of the American Heart Association.[1]
Overall, the study included a cohort of 271,804 patients who underwent transfemoral TAVR from 2017 to 2020. The mean age was 78.8 years old, and 55.8% of patients were men. All information came from the Nationwide Readmissions Database.
A Sentinel CPD was used in 7.3% of TAVR cases. The percentage of cases that included a CPD was just 0.8% in 2017, but that increased to 11.3% by 2020. Patients treated at metropolitan teaching hospitals were more likely to be treated using a CPD. In addition, the devices were more commonly used when patients had a bicuspid aortic valve, but they were less common when patients presented with atrial fibrillation (AFib), carotid artery disease, end-stage renal disease or prior coronary artery bypass grafting.
Tracking TAVR outcomes with and without the use of a cerebral protection device
The group had an overall stroke rate of 1.8% and a major stroke rate of 1.5%. Readmission rates were 11.6% after 30 days and 27.9% after 180 days. The median length of stay was 2 days.
Patients with a CPD were associated with lower stroke rate (1.6% vs. 1.9%) and lower major stroke rate (1.2% vs. 1.5%). Major strokes were defined as any stroke event that led to death or a nonroutine discharge.
CPD patients also had a lower mortality rate (0.7% vs. 1.3%) in addition to a slightly shorter median length of stay, more “routine discharges” and “significantly lower” readmission rates after 30 and 180 days.
Among TAVR patients who suffered a stroke, meanwhile, patients who underwent the procedure with a CPD got out of the hospital a full day faster on average. In-hospital death was also less likely if a CPD was used and a stroke occurred, though was not a significant difference in 30- or 180-day readmission rates.
Predicting stroke after TAVR
The Cleveland Clinic researchers noted that older patients and women were both linked to increased stroke risks after TAVR. A bicuspid aortic valve, AFib, carotid artery disease and end-stage renal disease on dialysis were also associated with a higher stroke risk. Prior valve surgery, meanwhile, appeared to make the greatest impact on a TAVR patient’s stroke risk.
Using a CPD, the team emphasized, “was not independently associated with lower stroke rates.”
Many of the same patient factors associated with a heightened stroke risk were also found to impact a patient’s risk of a major stroke. This included increasing age, female sex, a history of AFib and others. Again, prior valve surgery was the single biggest factor associated with increasing a patient’s risk.
One key difference, however, was that CPDs were independently associated with a lower major stroke risk than not using a CPD. The risk reduction was “modest,” the team wrote, but still strong enough to confirm a clear benefit.
“While patients with a CPD had lower overall stroke rates, this association was lost in the multivariable logistic regression model,” wrote first author Shashank Shekhar, MD, senior author Samir Kapadia, MD, and other co-authors from Cleveland Clinic. “These findings are consistent with a recent study from the Vizient database, which captures data from 400 U.S. academic centers, that also reported no significant reduction in post‐TAVR stroke rate with CPD use. However, a reduction was noted in major stroke, which is also consistent with findings from the large, randomized PROTECTED TAVR trial.”
Reviewing data from these various studies, the group wrote, appears to “reinforce the notion of a protective benefit of CPD use during TAVR upon major/disabling stroke, but not necessarily with the overall stroke risk.”
The authors did highlight the “challenging economic climate” for CBD devices due to increased costs and lack of reimbursement. Click here to read their full analysis.