ICE guidance reduces risk of permanent pacemaker implantation after TAVR with a self-expandable valve
Transcatheter aortic valve replacement (TAVR) with a self-expandable valve is associated with a heightened risk of conduction disturbances that lead to permanent pacemaker implantation (PPI). According to new research published in Circulation: Cardiovascular Intervention, however, utilizing the cusp-overlap method and intracardiac echocardiography (ICE) can help interventional cardiologists and the rest of the heart team limit such disturbances, keeping PPI to a minimum.
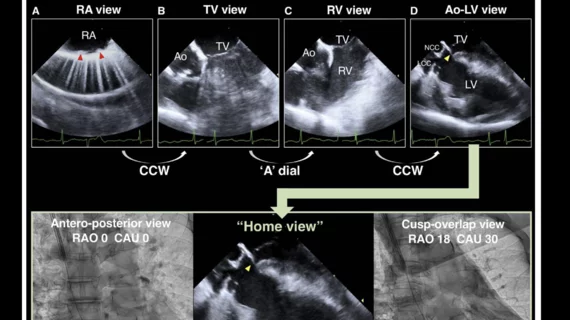
“The recently developed cusp-overlap method has been widely used in place of the conventional three-cusps method to achieve an accurate transcatheter heart valve (THV) implantation depth by eliminating the parallax between the aortic annulus and the delivery catheter,” wrote first author Kenichi Ishizu, MD, a cardiologist with Kokura Memorial Hospital in Japan, and colleagues. “However, the Optimize PRO study interim analysis, which examined the usefulness of the cusp-overlap method, reported a still relatively high PPI rate of 8.8%. Therefore, we utilized transjugular ICE to continuously monitor the membranous septum (MS) during TAVR and attempted to reduce the PPI rate by repositioning the device based on ICE findings.”
Ishizu et al. explored data from more than 1,500 consecutive TAVR procedures performed at the same facility from 2017 to 2022. After making certain exclusions, including patients who received a balloon-expandable THV, the group was left with 446 patients who received a self-expandable TAVR valve. The mean age was 85 years old, 76% were women and the median Society of Thoracic Surgeons risk score was 5.3. All patients received an Evolut R or Evolut PRO/PRO+ THV from Medtronic. Nearly all procedures were performed using the transfemoral approach, and nearly 60% involved a 26-mm THV.
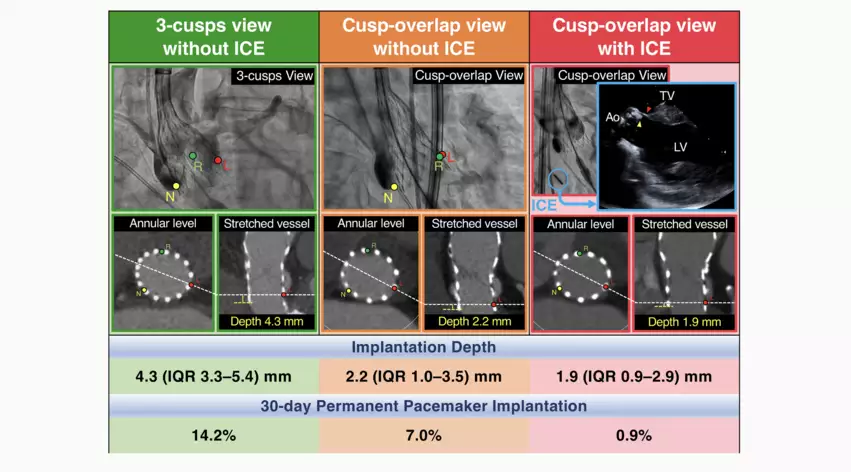
Comparing 3 different techniques for self-expandable TAVR
While the three-cusps method was used for 47.% of the study’s TAVR procedures, the cusp-overlap method without transjugular ICE was used for 28.9% and the cusp-overlap method with transjugular ICE was used for the remaining 23.8%. All patients underwent several 12-lead electrocardiograms after TAVR to track changes in conduction. If no significant changes were identified, and everything else proceeded as expected, the patient was discharged after five days.
Overall, these procedures were associated with a high technical success rate (98%) and device success rate (92.8%). All-cause mortality was comparable for all three groups. The median implantation depth was 4.3 mm for the patients treated with three-cusps method, 2.2 mm for patients treated with the cusp-overlap method with no ICE and 1.9 mm for patients treated with the cusp-overlap method with ICE.
New-onset conduction disturbances that led to PPI were seen in 9% of TAVR procedures after 30 days. These were due to high-degree atrioventricular block in three patients and complete atrioventricular block in another 37 patients. The 30-day PPI rate was much lower among patients treated with the cusp-overlap method and ICE (0.9%) than it was among those treated with just the cusp-overlap method (7%) or with the three-cusps method (14.2%). A separate analysis confirmed this new approach of using the cusp-overlap method and transjugular ICE was independently associated with a reduced PPI risk.
In addition, new-onset left bundle branch block (LBBB) was much more common among patients treated with the three-cusps method (39.3%) than patients treated with just the cusp-overlap method (24.8%) or the cusp-overlap method and ICE (24.5%).
“Our novel method combining the cusp-overlap view and ICE achieved a reliably higher THV position with a substantial reduction in the subsequent rates of PPI and conduction disturbances without compromising procedural safety and THV hemodynamics,” the authors wrote.
The group did note that their approach would increase healthcare costs, but they saw this as a potential long-term victory when it comes to lowering costs for the entire health system.
“The highly predictable avoidance of post-TAVR conduction disturbances by using ICE leads to a lower PPI rate and shorter hospital stays, which may have cost advantages,” they wrote. “In this scenario, it may be better for greater cost-effectiveness to apply our novel method selectively to patients at a high risk of post-TAVR conduction disturbances, such as those with baseline right bundle branch block and MS length < 2 mm.”
Read the full study here.
Click here to learn more about the growing role of ICE in today's evolving cardiology landscape.