New ‘zero-contrast’ TAVR technique shows promise in pilot study
A new approach to transcatheter aortic valve replacement (TAVR) that uses no iodine contrast material may be safe and feasible for patients who face a heightened risk of acute kidney injury (AKI) , according to a new analysis published in Frontiers in Cardiovascular Medicine.[1] The study’s authors focused on patients who present with severe symptomatic aortic stenosis (AS) and chronic kidney disease (CKD).
“AKI is frequently observed after TAVR, with rates ranging from 3% to 50% and up to 4.5% requiring dialysis,” wrote first author Antônio Fernando Diniz Freire, a researcher with the Heart Institute at the University of São Paulo in Brazil, and colleagues. “Of note, it may also occur in the pre-TAVR workup since the vast majority of such patients undergo contrast multidetector computed tomography (MDCT) evaluation. The occurrence of AKI has been related to the volume of contrast media used, in addition to the presence of comorbidities, such as CKD, which is commonly observed among TAVR candidates. It is noteworthy that AKI after TAVI is associated with poorer clinical outcomes, including a stepwise increase in all-cause death and cardiovascular mortality, according to AKI severity.”
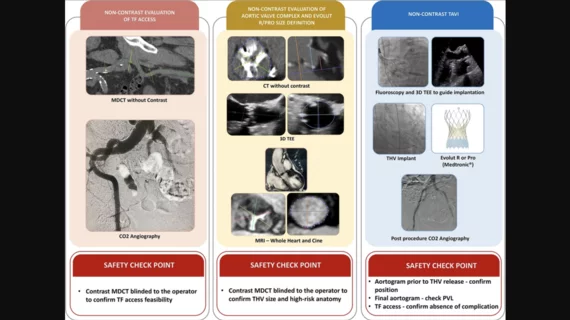
Freire et al. tracked data from 25 patients for their pilot study. All patients underwent transfemoral TAVR using this new “zero-contrast” technique from December 2020 to December 2021. They all received a self-expandable Evolut valve from Medtronic. Patients were excluded from the study if they were not suitable candidates for transfemoral access. Imaging modalities that do not use any contrast material were used to evaluate each patient before the procedure. However, contrast MDCT evaluations were still used just to confirm transfemoral TAVR was feasible and that the chosen heart valve was not undersized.
The mean patient age was 79 years old. Fifty-two percent of patients were men.
Overall, device success was 92%. Also, the study’s primary safety endpoint—being free of all-cause mortality, major stroke, life-threatening bleeding, AKI, coronary artery obstruction requiring intervention, major vascular complication or valve-related dysfunction after 30 days—was achieved in 92% of patients. There were no deaths or strokes after 30 days.
Also, in 36% of cases, the heart valve chosen for the procedure was one size larger than the one identified by the contrast MDCT evaluations.
“We believe that this new ‘zero-contrast’ technique for procedural planning and self-expandable transcatheter heart valve implantation might become the preferable strategy for a significant population of CKD patients undergoing TAVR,” the authors wrote. “Of course, the results of this pilot study deserve confirmation in a larger series to be implemented in clinical practice. Therefore, the next phase of the study using no contrast at all (without safety checkpoints) in a larger series of CKD patients is warranted.”
The authors did note that 24% of patients still ultimately presented with AKI. None of those patients required dialysis, however, and the group emphasized that “the main advantage of the present technique is not to expose patients to the nephrotoxicity of the contrast media.” Hypotension and inflammation were both listed as possible reasons these patients went on to develop AKI. Also, as previously mentioned, patients did still technically undergo a contrast MDCT evaluation.
This study was funded by a research grant from Medtronic. However, the authors wrote, Medtronic “was not involved in the study design, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.”
Read the full analysis here.