TAVR vs. surgery: Exploring 5-year outcomes among intermediate-risk patients
When treating intermediate-risk patients, transcatheter aortic valve replacement (TAVR) with a modern balloon-expandable heart valve and surgical aortic valve replacement (SAVR) are associated with similar five-year outcomes, according to new data published in the Journal of the American College of Cardiology.[1] The primary difference between the two treatments was the presence of paravalvular leak (PVL), which was more common after TAVR.
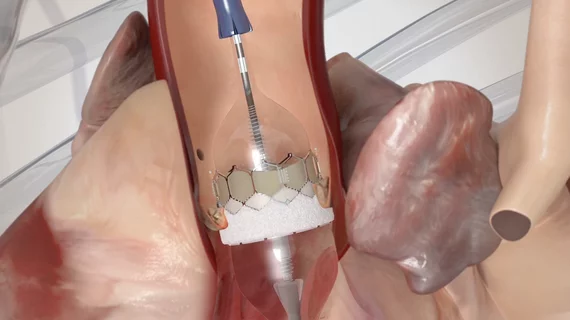
The study’s authors performed a propensity-matched analysis of 783 pairs of intermediate-risk patients with severe aortic stenosis. Each pair included one patient who underwent TAVR with a third-generation Sapien 3 TAVR valve from Edwards Lifesciences, and another patient who underwent SAVR. All patients were originally treated as participants in the Partner 2 S3 Intermediate or Partner 2A clinical trials. Clinicians performed follow-up clinical assessments on each patient at baseline and then again after 30 days, one year and annually for up to five years.
Overall, death or disabling stroke after five years were seen in 40.2% of TAVR patients and 42.7% of SAVR patients. Looking closer at stroke rates, nondisabling stroke was seen in 6.4% of TAVR patients and 3.5% of SAVR patients. Disabling stroke, meanwhile, was seen in 5.8% of TAVR patients and 7.9% of SAVR patients.
“Although overall stroke rates were not significantly different at five years, there were important differences in stroke severity,” wrote first author Mahesh V. Madhavan, MD, MS, with Columbia University Irving Medical Center and NewYork-Presbyterian Hospital in New York City, and colleagues. “The initial benefit in disabling stroke favoring TAVR was maintained at five-year follow-up. However, this was driven by the early events in the SAVR group, with no further difference in rates of disabling stroke between one and five years.”
The two treatment options were associated with comparable rates of additional five-year outcomes, including transient ischemic attack and rehospitalization.
Another key takeaway from this study was that, among patients with follow-up echocardiography results available, TAVR with the Sapien 3 valve was associated with higher rates of total aortic regurgitation and PVL at baseline and all follow-up points. When focused on moderate to severe aortic regurgitation and PVL, however, the team identified “no significant differences” between these two groups.
Madhavan et al. also noted that rates of moderate or greater structural valve deterioration-related hemodynamic valve deterioration and bioprosthetic valve failure after five years were comparable between TAVR and SAVR patients. Structural valve deterioration is an important topic when examining TAVR and SAVR outcomes, especially considering the recent trend of younger patients being considered for TAVR.
The authors concluded that more research is still needed on the long-term impact of TAVR.
“Additional studies with longer-term follow-up are required to provide better mechanistic insights regarding adverse clinical outcomes and bioprosthetic valve durability after aortic valve replacement with Sapien 3 TAVR compared with SAVR,” they wrote.
Co-authors for this five-year analysis included Martin B. Leon, MD; Samir Kapadia, MD; Rebecca T. Hahn, MD; Michael Mack, MD, John G. Webb, MD; Susheel K. Kodali, MD; and many other leading researchers in the world of TAVR.
Read the full study in the Journal of the American College of Cardiology here.