ACC consensus explains what cardiologists should look for in long COVID-19
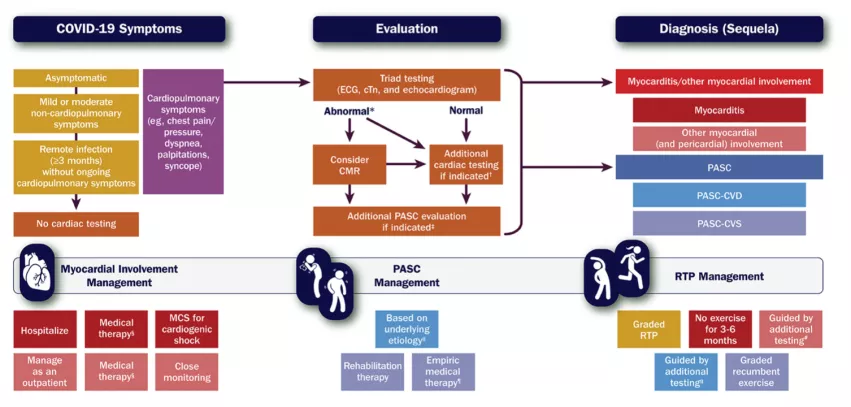
The American College of Cardiology (ACC) has issued a new expert consensus decision pathway for the evaluation and management of adults with cardiovascular consequences stemming from a COVID-19 infection. Over the past two years, numerous post-infection symptoms have been attributed to the effects of long COVID-19, also known by its official clinical designation as post-acute sequelae of SARS-CoV-2 infection (PASC). The ACC document discusses myocarditis and offers guidance for long COVID patients and on resumption of exercise and participation in sports after a COVID infection.
The clinical guidance “2022 ACC Expert Consensus Decision Pathway on Cardiovascular Sequelae of COVID-19: Myocarditis, Post-Acute Sequelae of SARS-CoV-2 Infection (PASC) and Return to Play” was published today in the Journal of the American College of Cardiology.[1]
“The best means to diagnose and treat myocarditis and long COVID following SARS-CoV-2 infection continues to evolve,” said Ty Gluckman, MD, MHA, co-chair of the expert consensus decision pathway and medical director of the Center for Cardiovascular Analytics, Research, and Data Science at Providence St. Joseph Health in Portland, Oregon. “This document attempts to provide key recommendations for how to evaluate and manage adults with these conditions, including guidance for safe return to play for both competitive and non-competitive athletes.”
Gluckman said the goal of the document is to provide guidance as physicians are trying to figure out how best to evaluate and manage these patients. As part of this document, Gluckman said they assembled a group of cardiac experts to create a framework to assist clinicians and to figure out the preferred ways to evaluate and managing patients presenting with symptoms that may track back to the cardiovascular system.
Overview of long COVID and its cardiovascular manifestations
Long COVID, or PASC, is a condition reported by 10-30% of infected patients. It is defined by a constellation of new, returning or persistent health problems experienced by patients four or more weeks after COVID-19 infection. The condition may manifest in widely disparate organ systems, and individuals can present with a range of symptoms that may be tracked in the cardiovascular system, Gluckman explained. The biggest symptoms of concern for cardiologists include myocarditis, tachycardia, exercise intolerance, chest pain, palpitations and shortness of breath.
“We recognize that often these individuals will present to their primary care clinicians seeking further evaluation and treatment, and many long COVID clinics have been created at medical centers across the United States,” Gluckman said, adding this is where most patients be be referred from for cardiac evaluations.
The writing committee has proposed two terms to better understand potential etiologies for those with cardiovascular symptoms:
• PASC-CVD, or PASC-Cardiovascular Disease, refers to a broad group of cardiovascular conditions (including myocarditis) that manifest at least four weeks after COVID-19 infection.
• PASC-CVS, or PASC-Cardiovascular Syndrome, includes a wide range of cardiovascular symptoms without objective evidence of cardiovascular disease following standard diagnostic testing.
The new guidelines suggest patients with long COVID and cardiovascular symptoms should undergo evaluation with laboratory tests, electrocardiograph (ECG), echocardiogram, ambulatory rhythm monitoring and/or additional pulmonary testing based on their clinical presentations. Cardiology consultation is recommended for abnormal test results, with additional evaluation based on the suspected clinical condition, especially myocarditis.
Myocarditis in long COVID PASC patients
Gluckman said myocardial and pericardial involvement is one of the biggest concerns post COVID so that was a primary focus in the document. “We do see cases of myocarditis as a rare manifestation after SARS-COVID-2 infection, These cases have been described well throughout the literature, since the pandemic began,” he said.
Myocarditis, or inflammation of the heart, is a condition defined by the presence of cardiac symptoms (chest pain, shortness of breath, palpitations), an elevated cardiac troponin (biomarker of cardiac injury), and abnormal electrocardiographic (ECG), cardiac imaging (echocardiogram, cardiac magnetic resonance imaging, or fluorodeoxy-glucose (FDG)-PET) and/or cardiac biopsy findings. Gluckman said very aggressive manifestations myocarditis can involve conduction heart block, cardiac shock and severe compromise of left ventricular ejection fraction.
“The time course for myocarditis can often develop weeks after their original infection, so it's not inconsistent to have someone who presents weeks or a month plus after their original infection. And in fact, myocarditis is the underlying condition that is responsible for some symptoms of long COVID,” Gluckman explained. “That being said, I do want to reassure individuals that the vast majority of individuals with long COVID do not have myocarditis. But as part of the basic evaluation that we outlined from a cardiovascular standpoint, that may be done by a primary care clinician.”
Although rare, myocarditis with COVID-19 is more commonly seen in men. Because myocarditis is associated with a higher risk of cardiac complications, a proactive management plan should be in place to care for these individuals, the ACC said. For patients with mild or moderate forms of myocarditis, hospitalization is recommended to closely monitor for worsening symptoms, while undergoing follow-up testing and treatment. The consensus document says patients with severe myocarditis should ideally be hospitalized at centers with expertise in advanced heart failure, mechanical circulatory support and other advanced therapies.
Management of myocarditis caused by COVID vaccines
Myocarditis following COVID-19 mRNA vaccination is very rare, the ACC document stated, but a section was included for the management of these patients. As of May 22, 2021, the U.S. Vaccine Adverse Event Reporting System (VAERS) noted rates of 40.6 cases per million after the second vaccine dose among male individuals aged 12-29 years and 2.4 cases per million among male individuals over the age of 30. Corresponding rates in female individuals were 4.2 and 1 cases per million, respectively.
Although most cases of myocarditis following COVID-19 mRNA vaccination are mild, the consensus document suggests these patients should be diagnosed and treated similarly to those with myocarditis following a COVID-19 infection. The document also states that currently approved COVID-19 mRNA vaccines are highly effective, and the benefit-to-risk ratio is very favorable across all demographic groups.
The document includes a risk vs. benefits figure based on data from the Centers for Disease Control and Prevention (CDC). It states that, for every 1 million COVID-19 mRNA vaccinations in males 12-29, it is expected there will be about 39-47 more cases of myocarditis. However, on the benefits side of the scale, these vaccinations help prevent 560 fewer hospitalizations, 138 fewer ICU admissions and 6 fewer deaths.
Guidance on athletes returning to play after COVID infection
The ACC said the observation of cardiac injury among some patients hospitalized with COVID-19, coupled with uncertainty around cardiovascular sequelae after mild illness, fueled early apprehension regarding the safety of competitive sports for athletes recovering from COVID-19 infection. However, subsequent data from large registries have demonstrated low prevalence of clinical myocarditis, and there has not been a rise in adverse cardiac event rates. The updated ACC guidance includes a practical, evidence-based framework to guide resumption of athletics and intense exercise training.
For athletes recovering from COVID-19 with ongoing cardiopulmonary symptoms (including chest pain, shortness of breath, palpitations, lightheadedness) or those requiring hospitalization with increased suspicion for cardiac involvement, further evaluation should use triad testing, which includes an ECG, cardiac troponin and an echocardiogram. For those with abnormal test results, the guidance document says further evaluation with cardiac MRI should be considered.
Avoid bedrest and not exercising to prevent worsening long COVID
For patients with tachycardia and exercise intolerance, increased bedrest and/or a decline in physical activity may trigger cardiovascular deconditioning with progressive worsening of symptoms, the document warns.
“There appears to be a ‘downward spiral’ for long COVID patients. Fatigue and decreased exercise capacity lead to diminished activity and bedrest, in turn leading to worsening symptoms and decreased quality of life,” said Nicole Bhave, MD, co-chair of the expert consensus decision pathway said in an ACC statement about the publication of the guidelines “The writing committee recommends a basic cardiopulmonary evaluation performed upfront to determine if further specialty care and formalized medical therapy is needed for these patients.”
For PASC-CVS patients with tachycardia and exercise intolerance, upright exercise (including walking or jogging) should be replaced with recumbent or semi-recumbent exercise (such as rowing, swimming or cycling) to avoid worsening fatigue. Exercise intensity and duration should be low initially, with gradual increases in exercise duration over time. Transition back to upright exercise can be done as a patient's symptoms improve. Additional interventions, including increased salt and fluid intake, elevation of the head during sleep, support stockings and pharmacological treatments such as beta-blockers should also be considered on a case-by-case basis, the document states.
Long COVID can cause arrhythmias
Long COVID clinics have identified arrhythmias as one of the top presentations in PASC patients, including atrial fibrillation (AFib). In some of these cases involving younger patients, testing shows these patients were predisposed to AFib and likely would have developed it later in life, but the COVID infection brought on early onset.
“It may well be that the pandemic, specifically in SARS-COVID-2, infection may uncover an individual that otherwise had a pre-existing condition that we didn't otherwise appreciate,” Gluckman said. “It's also possible that the virus itself may trigger through various different mechanisms that lead to the development of certain forms of cardiovascular disease that may not have predated their infection, but actually developed subsequent to it. I think it's fair to say that individuals that have symptoms consistent long COVID, or PASC, are likely to fit into one of these two categories.”
The document outlines specific testing and symptoms in long COVID patients, especially as it related to exercise.
Anyone diagnosed with clinical myocarditis should abstain from exercise for three to six months.
The ACC guidance states cardiac testing is not recommended for asymptomatic individuals following COVID-19 infection. Individuals should abstain from training for three days to ensure that symptoms do not develop. For those with mild or moderate non-cardiopulmonary symptoms (fever, lethargy, muscle aches), training may resume after symptom resolution. For those with remote infection (≥ three months) without ongoing cardiopulmonary symptoms, a gradual increase in exercise is recommended without the need for cardiac testing.
Based on the low prevalence of myocarditis observed in competitive athletes with COVID-19, the authors note that these recommendations can be reasonably applied to high-school athletes (aged ≥14 years) along with adult recreational exercise enthusiasts. The authors of the document said future study is needed to better understand how long cardiac abnormalities persist following COVID-19 infection and the role of exercise training in long COVID.
“Early on when the pandemic first hit, we recognized that there were fair numbers of individuals being hospitalized, and in fact, they would have elevated troponin levels consistent with myocardial injury.” Gluckman said, which led to the creation of registries for long-term tracking these patients. “But the registry data provides a level of reassurance that the rates of clinical myocarditis among athletes is less than 1%. So the overwhelming majority of individuals that are infected with SARS-COVID-2 are unlikely to manifest clinical myocarditis.”
He said the guidance document offers a number of different paths based on whether someone has asymptomatic COVID infection or symptoms associated with an infection The pathways can also help determine if they suffer from a cardiopulmonary etiology with symptoms, such as chest discomfort, shorter shortness of breath, light headedness, palpitations, or whether they have non-cardiopulmonary symptoms such as fever and muscle aches.
Future directions for cardiac long COVID studies
Gluckman said data is still being gathered on post-COVID conditions and there might be impacts from different variants of the virus. The document states little is also currently known about the incidence of PASC in children, patients who experience a vaccine breakthrough infection, or those affected by newer SARS-CoV-2 variants, including Delta and Omicron. The document also underscores the need to conduct additional studies to define best practices for distinct phenotypes.
ACC.22 session will explain the new long COVID cardiology management guidance document
The 2022 ACC expert consensus on PASC and return to play will be discussed in a session at the ACC’s 71st Annual Scientific Session on April 3 at 4:30 p.m. ET. Learn more about the session.
Related COVID-19 Content:
Athletes with COVID-19 may require heart MRI screening for myocarditis, new data suggest
4 cardiac arrhythmias associated with COVID-19
What we know about COVID-19 and cardiogenic shock
Mild COVID-19 infections not associated with long-term risk of heart damage
The pandemic’s toll: 55 long-term side effects of COVID-19
4 key takeaways from an updated look at vaccine-related myocarditis in the U.S.
Most young people with vaccine-related myocarditis recover quickly
Intrathoracic complications in COVID patients: Incidence, associations and outcomes
Congenital heart disease increases risk of poor COVID-19 outcomes, including death
MRI scans show COVID's 'significant' impact on the brain
Heart complication seen for the first time in a young patient after COVID-19 vaccination
American Heart Association investing $10 million to study the long-term consequences of COVID-19
Cardiologist discusses COVID-19, myocarditis among professional athletes and more
Not so fast: Specialists warn against cardiac imaging for asymptomatic COVID-19 patients
Study shows COVID-19 can infect heart cells—and do serious damage in the process
ACC issues COVID-19 guidance for cardiologists
New imaging evidence may link myocarditis in young adults to COVID-19 vaccination
Reference: