Time running out to comment on higher cardiac CT payments
Public comments on the Centers for Medicare and Medicaid Services (CMS) proposal to double payments for cardiac computed tomography (CT) exams are being accepted until Monday, Sept. 9.
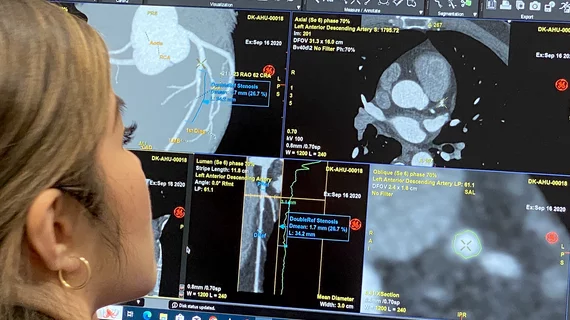
Cardiac CT experts are saying the move could reshape the financial landscape for hospitals offering this diagnostic service. While cardiac CT has seen significant growth in the past few years, Medicare payments do not cover the full cost of the procedure. This has been a barrier to wider expansion, especially for heart teams working out of smaller centers.
The recently released 2025 Medicare Hospital Outpatient Prospective Payment System (HOPPS) proposed rule might raise Medicare reimbursement for CCTA from $175 to $386 by moving it to a new ambulatory payment classification (APC). The Society of Cardiovascular Computed Tomography (SCCT) said historically, Medicare Administrative Coordinators (MACs) have restricted hospitals to using the radiology CT revenue code (0350) for CCTA instead of the higher-paying cardiology code (0480). SCCT said CMS addressed this issue via a transmittal earlier this year, but other payer and clearinghouse edits still require the CT revenue code, preventing the use of the cardiology revenue code.
CMS is seeking comments to ascertain whether 50% or more hospital outpatient departments are using, have attempted to use, or would use a revenue cardiology code for CCTA tests if allowed.
"CCTA has been severely under-reimbursed for years. The increased reimbursement would have huge implications and would alleviate financial pressure on medical practices. Consequently, a higher payment rate could lead to cardiac CT testing being offered at more sites, ensuring better patient access to this cost-efficient exam," SCCT explained in a statement on its advocacy page for this change.
Currently, hospitals must submit charges under general radiology or CT revenue codes, which undervalue the procedure, explained Ron Blankstein, MD, associate director of the cardiovascular imaging program and director of cardiac CT at Brigham and Women’s Hospital, and a former SCCT president. He said the proposed CMS changes would allow hospitals to use cardiology-specific revenue codes, potentially leading to higher payments. However, there were some barriers to billing under cardiology versus radiology.
"What CMS is now saying is they want to hear from hospitals and if they hear that more than 50% of cardiac CT exams potentially could be charged under a different revenue code, they are willing to entertain moving cardiac CT to a different APC. So what this means is, hospitals need to share their experience with CMS about which revenue code they're using and why they haven't switched to cardiac CT revenue codes," Blankstein explained.
He said hospitals responding to CMS should describe some of the obstacles they face, and at least express that they have an interest in switching cardiac CT charges to a different revenue code.
Comments can be submitted directly to CMS here.
Watch a video interview with Blankstein explaining the details of why CMS is considering the increase and how cardiac is currently reimbursed: Higher payments for CCTA could bring considerable change to cardiology.