Medicare coverage for weight loss drug semaglutide could cost up to $145B per year
Medicare’s decision to cover semaglutide, the first weight loss drug approved by the U.S. Food and Drug Administration (FDA) to reduce heart risks, could end up increasing healthcare costs by billions of dollars, according to new research published in Annals of Internal Medicine.[1]
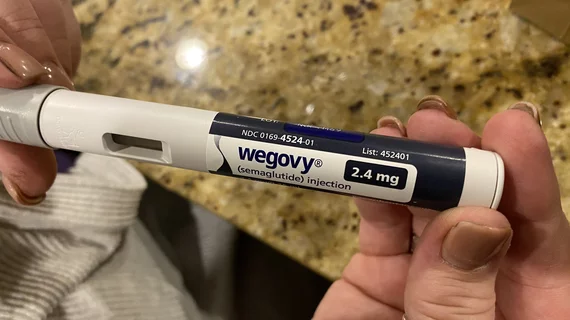
Semaglutide is a GLP-1 receptor agonist originally developed to treat diabetes. Novo Nordisk sells and markets its weekly subcutaneous treatments of semaglutide 2.4 mg under the brand name Wegovy, and interest in the drug skyrocketed after the FDA’s decision.
Back in March, the U.S. Centers for Medicare and Medicaid Services (CMS) announced Medicare would cover Wegovy if prescribed to patients with an elevated body mass index (BMI) and established cardiovascular disease (CVD). The team behind this new analysis aimed to evaluate how much the CMS decision could impact healthcare costs in the years ahead, exploring data from the National Health and Nutrition Examination Survey.
Overall, they estimated that approximately 3.6 million people could be newly eligible to being prescribed Wegovy—and that could jump all the way to 15.2 million people if a more liberal definition of CVD is implemented. This would increase annual Medicare spending by $34 billion or $145 billion, respectively, the group wrote.
“When established CVD is narrowly defined, only one in seven Medicare beneficiaries with elevated BMI are likely to be eligible to receive semaglutide, but costs to Medicare could still exceed $10 billion per year,” lead author Alexander Chaitoff, MD, MPH, a researcher with the Center for Healthcare Delivery Sciences at Brigham and Women’s Hospital, said in a statement. “In this conservative coverage scenario, that means most beneficiaries with elevated BMI and cardiovascular risk would remain ineligible for semaglutide, yet the medication could still potentially become one of the costliest drugs to Medicare.”
The high costs associated with semaglutide have been researched at length as the drug has gained popularity. According to a March 2024 analysis by the Congressional Budget Office, the drug is expected to be included in future CMS price negotiations.
Click here to read the full research letter in Annals of Internal Medicine, an American College of Physicians journal.