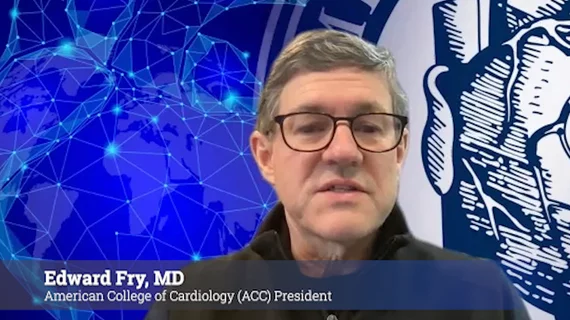
Q&A: New ACC President Edward Fry discusses the past, present and future of cardiology
Edward T.A. Fry, MD, officially became the new president of the American College of Cardiology (ACC) at the close of ACC.22 in Washington, D.C. Fry, a longtime ACC member, currently serves as an interventional and general cardiologist at Ascension St. Vincent Heart Center in Indianapolis.
Fry spoke with Cardiovascular Business about a wide variety of topics, including the ACC’s successful return to in-person meetings, some helpful ways to address physician burnout and his biggest goals for the next year.
Read below for our full conversation:
Cardiovascular Business: It’s been a challenging few years for cardiologists. How does it feel to begin your term as ACC president just as in-person conferences are returning and specialists are once again able to meet and communicate in person?
Edward Fry: Yeah, it was a great experience. Not to make a pun, but it was just what the doctor ordered.
It was a real shot in the arm for everybody. People were really desiring that person-to-person contact and communication, which is obviously just not replicable over video.
We’ve learned so much in terms of what capabilities there are and what technology can do, but it can't substitute for human interaction. It was very reassuring to see that the ability to talk to one another supports creativity and makes conversations easier.
Cardiovascular Business: During your speech at the end of ACC.22, you noted that cardiologists and their care teams have learned a lot during the pandemic about how to reach patients and improve care. Can you speak about some of those lessons?
Edward Fry: There were a lot of things pre-pandemic that were impending challenges — access, availability, follow-through communication — and we had had to solve those immediately, so that’s what we did. Leveraging telehealth, remote patient monitoring and those different ways of communicating became very necessary and helpful. I am glad we learned how to do these things to accommodate patients during the pandemic.
As you are well aware, in those first couple of weeks, we went from essentially zero telehealth to 90% telehealth. And then as things kind of backed off, we slid back pretty quickly to about 10% or so telehealth. There were a lot of drivers of that. The patients wanted it, and I think the providers wanted it too. The payment systems were geared toward that. Our workflows and the way things were set up, they were also geared toward that. That may be an opportunity we still have to build upon.
During this time, we also saw a lot of innovation and technology development in terms of patients be able to collect data on their own at home. We were even conducting clinical trials through totally virtual platforms. Those capabilities are here to stay, we just have to figure out the best way to integrate them into our workflows and take full advantage of them.
Cardiovascular Business: The ACC has started focusing more and more on ways to improve health inequities. Can you speak for a minute about why this is so important?
Edward Fry: Well, the first thing is recognition; you can't solve the problem if you don't recognize it. Although there was certainly some lip service given to it pre-pandemic, the realities of it became so obvious [once the pandemic started].
When you saw the disparities in access to care, in quality of care, in the type of care — and the differences in outcomes and mortality — just very rapidly and explicitly demonstrated by COVID-19, and you saw the healthcare systems’ flaws in terms being able to meet these demands, it all became so obvious. There were also many things that were not rocket science that could remedy some of those things — they just hadn't been done. Looking at access, improving advocacy, thinking about equality, thinking about a patient's right to expect that they can have the best and fullest outcome with respect to their healthcare. All of these things came together.
We are nowhere near declaring victory or anything like that. But just the simple recognition that we have a long way to go and a lot of problems to solve has exposed other underlying issues such as disparities in education, disparities in income, disparities in environment and racism. All of those things are big, big issues.
You have probably seen the statistics and the graphics that say a patient's true outcome with respect to their health is as little as 20% a direct result of the traditional clinical care we deliver. Eighty percent comes from these other social determinants that we have to learn how to reach into and affect in addition to practicing medicine.
Cardiovascular Business: I also wanted to get your thoughts on the ongoing issue of physician burnout. Why do you think this continues to be an issue in cardiology and other specialties?
Edward Fry: This is another problem that existed before the pandemic, but the statistics show that the incidents of burnout and the severity of burnout doubled during the pandemic, and that’s not surprising in the least. There were great clinical demands placed on the entire cardiovascular team at the time, not just the physicians, but nurses, technicians, administrators, everybody.
With the intensity of the medical illness, the limitations of resources, the pressures of time, the physical burden, the physical threats — early on, we didn’t even know if you’d die if you walked in the hospital to take care of somebody — it was a very scary situation. So that’s one part of it. Some things that had started beforehand were a sense of disengagement and a feeling that perhaps we've lost a little bit of our professionalism, which really is defined by self-governance, and self-responsibility.
Part of that was perhaps magnified in cardiology, where we had a huge shift from 90% of cardiologists being independent or in an academic practice, to today, when 80% of cardiologists are employed. That great change sort of peaked in 2008 or 2010, so we now have half a generation of cardiologists who have probably never experienced things other than employment. From that mindset may come a sense that they don't have a control over their profession and their environment, and that's a big driver of burnout. One remedy for that is to become engaged and to take charge. But that takes effort and time, and it sometimes becomes a paradox where, to have more control, you have to exert more effort and time. But that’s the definition of professionalism.
The last piece is personal resilience. That’s an area where I think some things are being done, like getting state licensing boards to remove questions related to personal mental health that people often don't answer honestly from licensing or credentialing documents. Instead, normalize a situation where it's OK for people to say, “I have stress, I have difficulty, I'm not coping well, I need help.” That's a much healthier environment than trying to just put a veneer on something and cover it up. So I think the ACC is doing things to address these problems through advocacy and through giving people the tools to be engaged effectively.
Cardiovascular Business: Do you think leaders play a pivotal piece here? You mentioned that people may feel like they can't always be honest when they're answering questions about mental health. Does that improve if administrators and other leaders all change the way they communicate?
Edward Fry: Oh yeah, absolutely. There’s this expectation of the stiff upper lip and, you know, that you can’t admit any perceived weaknesses. That very much comes from leadership, and leaders have a great opportunity to correct that and create a culture and an environment where it's OK to think about those things.
ACC President Edward T.A. Fry, MD, discusses burnout in cardiology.
Cardiovascular Business: What are some technologies or breakthroughs in cardiology you are especially excited about right now? What did you see at ACC.22 that is sure to make a big impact?
Edward Fry: There was a whole cornucopia of things at ACC.22, from technology to basic science, from pharmacology to devices, from procedures to epidemiology. It was great to have that all in one place. And again, going back to your original question about the meeting, it was so great to have those immediate reactions, to bounce your impressions off your colleagues and deal with that in a very human and interactive way.
Substantively, I think there are a couple big things like the rapid evolution of advanced imaging technologies and the amazing technology, techniques and skills related to structural heart work. But probably the important thing is the better understanding of preventive therapies that are effective. What are things that have a long-lasting impact and really pay it forward? That's really the basis of value-based care. I think that was the biggest thing I took away from the meeting.
Cardiovascular Business: What’s your biggest goal for your time as the president of the ACC?
Edward Fry: Well, No. 1 is to get out of the way of people who are a whole lot smarter than I am and put their energies and talents to good use. We really are at a critical juncture in healthcare, not just cardiovascular care, but everywhere. I think cardiovascular medicine has great tools to be able to address that by delivering on the transformation of care and really changing in a fundamental way how we deliver care, how we value care, and how we leverage innovation and technology to deliver on that quadruple aim of improved access, better outcomes, better experience and professionalism.
It goes back to the engagement piece. If we get people excited to do the right thing, show them that there is a reward for doing the right thing and change the incentives in the correct way, I think we can address a lot of those things together. Lastly, with the recognition of the equity piece and how healthcare really has to fit into this global approach that includes social determinants of health, I hope that leveraging all the assets that we have in ACC — advocacy, science, education, publishing, discovery, leadership development — can give people the tools they need to truly deliver on transformation.
More video interviews with ACC president:
VIDEO: Factors causing cardiologist burn out — Interview with ACC President Edward Fry, MD
VIDEO: ACC president shares his technology takeaways at ACC 2022
VIDEO: ACC President Edward Fry outlines disparities in care seen during the pandemic
Related ACC.22 Content:
Links to the ACC.22 late-breaking clinical trials
TAVR vs. surgery, FFR-guided PCI and DCB safety: Day 3 at ACC.22
Cholesterol medications, flu shots and heart failure: Day 2 at ACC.22
Salt restrictions, PCI breakthroughs and a social media primer for cardiologists: Day 1 at ACC.22
VIDEO: TAVR durability outperforms surgical valves
Key interventional cardiology takeaways from ACC.22
VIDEO: MitraClip vs. surgical mitral valve replacement
Renal denervation linked to significant blood pressure reductions after 3 years