Targeting Unnecessary Practice Variation: A Conversation About Quality, Cost & Becoming a High-reliability Organization
Is practice variation a real problem or a passing trend? Which metrics matter? Are there practical approaches healthcare leaders should use to tackle variation and, if so, how can they get their teams on board? Cardiologists and administrators weigh in.
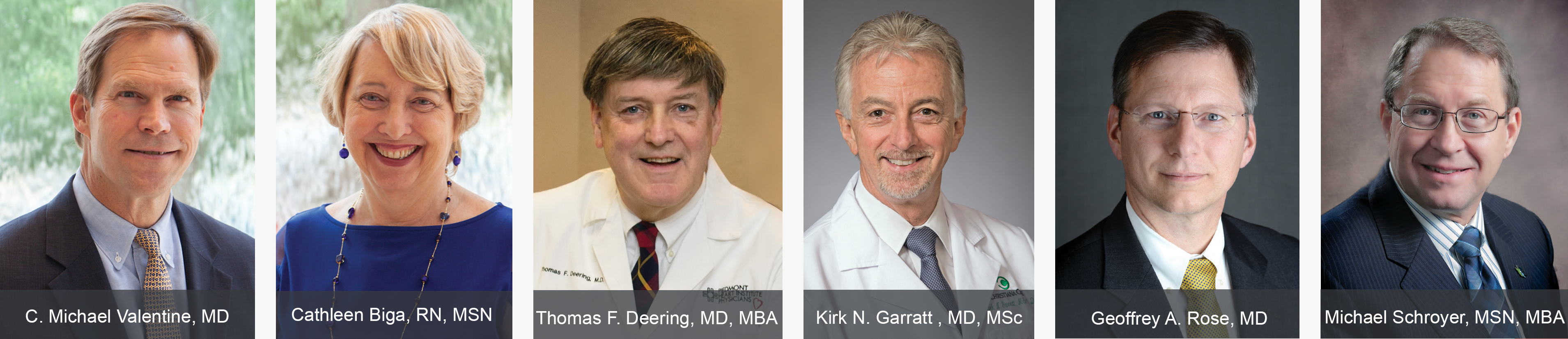
ROUNDTABLE PARTICIPANTS
- Thomas F. Deering, MD, MBA—2018-2019 President, Heart Rhythm Society; Mark E. Silverman, MD, Educational Chair and Clinical Associate Professor of Medicine, Medical College of Georgia; Chief Quality Officer and Chief of the Arrhythmia Center, Piedmont Heart Institute, Atlanta
- Kirk N. Garratt , MD, MSc—2017-2018 President, Society for Cardiovascular Angiography and Interventions; John H. Ammon Chair of Cardiology and Medical Director, Center for Heart and Vascular Health, Christiana Care Health System, Newark, Del.
- Geoffrey A. Rose, MD—2018-2019 Member, Board of Directors, American Society of Echocardiography; Chief, Division of Adult Cardiology, Sanger Heart & Vascular Institute, Atrium Health, Charlotte, N.C.
- Michael Schroyer, MSN, MBA—Regional President, St. Vincent Northeast Region, St. Vincent Health, Ascension, Indianapolis
ROUNDTABLE MODERATORS
- C. Michael Valentine, MD—2018-2019 President, American College of Cardiology; Senior Cardiologist, Stroobants Cardiovascular Center, Centra Health, Lynchburg, Va.
- Cathleen Biga, RN, MSN—American College of Cardiology Trustee; Chief Executive Officer, Cardiovascular Management of Illinois, Woodridge
When the American College of Cardiology (ACC) convened its 2018 Cardiovascular Summit and Leadership Forum in February, the session that generated the most comments—and the greatest demand for more discussion, according to program organizer and Cardiovascular Business editorial advisor Cathleen Biga, RN, MSN—was a panel discussion about unnecessary practice variation. Moderated by C. Michael Valentine, MD, an invasive cardiologist at Centra Health in Lynchburg, Va., the session featured speakers from the Heart Rhythm Society and the Society for Cardiovascular Angiography and Interventions.
CVB takes up the conversation here, welcoming Valentine, now the ACC’s president, and Biga as moderators, along with participants representing electrophysiology, interventional cardiology, noninvasive cardiology and hospital administration. In the following excerpts, they discuss the challenges inherent in differentiating between appropriate and unnecessary practice variation and share insights they’ve gleaned from tackling variability in their own health systems.
FIRST, TAKE STOCK: IDENTIFY UNNECESSARY VARIATIONS & UNDERSTAND THE CAUSES
VALENTINE: In discussions like this one, it’s key to start by agreeing on what we mean by unnecessary practice variation and clarifying whether we are focusing on quality or cost. The methodology is clearer for quality, so let’s begin there. How do you identify unnecessary practice variations as they relate to quality?
ROSE: At the Sanger Heart & Vascular Institute, we approach it through three frameworks. The first and most common is overuse. Are there practices that are no longer in keeping with accepted best practice, through either guidelines or appropriate care? What vestiges of old practice do we need to unlearn or sunset? That’s the first target—taking a really hard look at opportunities to stop doing things we don’t need to do any longer because of current science and state of practice.
The second area is underuse, which might get a little less attention. We have to ask ourselves, are there evidence-based practices that we are not systematically integrating into care pathways? We all know the axiom that it takes 17 years to bring and embed a practice into clinical practice.
The last area is methodologic variation. For example, not embracing radial access in the cath lab even though we know there may be clinical advantages to patients but, because it’s a newer approach, some practitioners may be slower to adopt. It’s not that other ways are wrong, but perhaps there’s a better way.
BIGA: Do you think practice variation is a real problem for healthcare, or is it a flash in the pan?
ROSE: It’s the major challenge we’re facing today in American medicine. I don’t think it’s going away nor do I think it should. We have improved outcomes tremendously, but it has come at a cost. We must be able to rigorously look at the things we do and find deficiencies that we know are there. And I mean the deficiencies that will be uncovered through the same data-based approach that we use to identify new therapies in the first place.
BIGA: That brings us to evidence-based guidelines. How important are they in looking at variations?
GARRATT: Historically, practice variation has been wrapped up in uncertainty about what to do. But, in the past 30 or 40 years, randomized trials have allowed us to be more definitive about what works and what doesn’t work, what’s best and what isn’t best. Once you bake that knowledge into performance standards or practice guidelines that are vetted by thought-leaders and respected practitioners, then they will be adopted by the majority. Th at’s what allows unnecessary and unwanted practice variation to be meaningfully reduced.
Today unnecessary practice variation comes in a couple of different forms. First is resistance, reluctance or hesitance about certain guideline standards being ideal for your patients. It’s a diminishing issue, but it still lingers. Second is what to do with those patients for whom we don’t have definitive practice standards based on randomized trials. That still applies to a large cut of the patients we serve.
BIGA: Have you found registry data to be useful for looking at variations in care and drilling down to individual practitioners? Or are you using registry data in other ways?
GARRATT: At Christiana Care Health System and, in fact, all three organizations that I’ve worked with in my career, we have leaned on registry data to help us understand where we stood in the landscape of clinical practice. This has been most important in the cath lab, but with the availability of broader registries and other sources of benchmarking information, the approach has proved itself to be useful in determining whether our practice is in the middle of the pack or at one extreme or the other. The value of the registries is not going to diminish importantly going forward because we’re all interested in having a sense of where we stand.
DON’T BE TOO RIGID: CONSIDER PHYSICIANS’ CONCERNS & ALLOW SOME VARIABILITY
VALENTINE: We’ve heard two service line directors speaking about unnecessary variation. Dr. Deering, how do you look at this question from the perspective of an electrophysiologist and the Heart Rhythm Society president? What is the usual response of practicing physicians?
DEERING: The response is evolving. Five or 10 years ago, the typical response of a clinician would be to justify his or her own approach and to not want to be told how to do things. Fortunately, today, we are in a different world. We realize we have limited resources, that quality care is exceedingly important and, when we are provided with data that show we can do a better job, clinicians want to get on board.
There will always be physicians who question, so part of the Heart Rhythm Society’s goal is to make sure that we get accurate data, analyze it and ensure that institutions and clinicians are looking at the data positively, in a carpe diem sense. By that I mean taking charge and wanting to lead the drive so that we can determine the course of action that results in better patient care, as opposed to having it handed to us.
BIGA: If we could eliminate some of the unnecessary variation in clinical care, would it affect our costs?
SCHROYER: We would see a great impact on the overall cost. I’ve seen that at St. Vincent Health and other cardiovascular entities I’ve been involved with. As we’ve looked at our data, we’ve been able to decrease our overall costs.
If you have several cardiologists doing various things differently, you will add to your cost just to make sure you have everything according to the order sets that each clinician is using. When everybody agrees to one order set for a condition, you can greatly decrease your cost through efficiency and reduced supply and equipment cost.
Here’s an example of something we’ve done that, importantly, our cardiologists led. The cardiologists got together and looked at the data and best practices and then decided which pacemakers, stents, catheters, balloons and so on that we would use. Just by reducing the variety of devices we use, our overall cost fell substantially. At our heart center, we’re able to do everything at very low cost, and it has proven to be enormous for us—for our bottom line, yes, but also for our quality.
VALENTINE: ACC data now show that 74 percent of members are employed. In fact, each of you is part of a system with employed cardiologists. Is employing physicians a problem or a boon for reducing unnecessary variability?
ROSE: It’s a real boon, but it depends on the communication strategies we use. Most people will accept that variation equals cost, and we all know that healthcare has a cost problem. So, out of the gate, most physicians accept this.
But at the same time, we also recognize that we’re taking care of patients and every patient is a little bit different. That’s why it becomes a conversation around constraining variation, not elimination of all variation. We ask, what is the acceptable degree of variation within a service line around a particular disease state or a particular procedure? When it’s framed in those terms, it’s much more comfortable to our colleagues. And being in a system-based model allows those conversations to move efficiently and effectively.
SCHROYER: You have to allow some variability within standard order sets. You keep track of it and, if you see a trend, then go back and take a look. Yes, patients are different, but at least we have guidelines. It’s wise to accept a little variability but also to track and monitor it.
PROVIDE USABLE TOOLS: ADOPT ORDER SETS & PATHWAYS
BIGA: Let’s dig a little deeper on order sets because, in my experience, they’ve been a challenge. How do physicians feel about the consistent use of order sets? Could they truly move us toward the triple aim? Or even the quadruple aim—if they took some of the burden off of physicians?
GARRATT: At our institution, the reaction to standardized order sets for cardiology disease states has been varied. The chest pain series has been relatively well embraced. Heart failure, on the other hand, has been more difficult. Part of that’s wrapped up in the fact that not all heart failure patients are cared for by cardiologists. There’s a strong need to educate not just your cardiovascular practitioners but your hospitalists, internists and others who may be caring for heart failure patients in the inpatient setting.
Once you get past the challenge of familiarizing people with the order sets and getting them to try them, for the most part people like them. Order sets simplify the admission process, and everyone loves that. Order sets also generally ensure everything that needs to get done is done for each patient. That is, after all, the principle aim of a standardized order set. And they help you get things done efficiently.
With order sets, practitioners tend to receive positive feedback for having reduced lengths of stay, for doing the right things to prevent readmissions and so on. Once the education piece has been done and clinicians try them, as long as they’re structured to be used without too much difficulty, they’re well accepted.
VALENTINE: It sounds like there is a real opportunity here for communications from medical society leadership.
DEERING: There is a great opportunity for societies to frame the message. Along those lines, there’s a secondary opportunity. Ideally what effective order sets do is engage all clinicians—residents and fellows, attending physicians, advanced practice providers, nurses, dieticians and so on. Wherever they’re relevant to clinical practice, order sets can be used as foundational pathway tools to deliver better patient care.
These are the things that will significantly reduce variation and, outward from that, yield better quality and lower cost, which will lead to higher value. As societies, we need to be not just creating guidelines—we’ve done a wonderful job with that. Not just creating physician papers—we’ve done that. We also need to give those documents life, so that they become the way we practice, not just something that sits there and informs us.
ROSE: There’s a place and a space here for pathways beyond guidelines. The guidelines and appropriate care documents give us an array of choices around a common condition; however, local expertise and local resources really must factor into how to deliver care in a local environment. For example, we have a patient presenting with chest pain in the outpatient setting. We could talk about nuclear cardiology as an appropriate approach, but then again cardiac CT might offer an advantage. What each of us will choose to do will be a function of the expertise and resources we have in our local environment.
So, in that local environment, can we constrain the variation of approach so that the practitioners are tackling that problem in a common way? Th at’s where pathways come into play. There is a real opportunity at the service line level to condense the guidelines, translate them into local pathways that capitalize on the local resources and expertise. That’s a conversation that needs to be elevated.
BIGA: Is pathway development where the rubber hits the road? Dr. Garratt, are you using pathways in your organization, and, if so, are they embraced by both employed and independent physicians?
GARRATT: Three years ago, our senior leadership challenged all of the service lines to produce at least one clinical pathway for a common disease state. We developed a pathway for non-ST-segment-elevation myocardial infarction. The goal was to contain unwanted clinical care variation, and there was an expectation that the pathway would reduce lengths of stay, readmission rates and costs. For the most part, our pathway worked, and the other service lines’ pathways enjoyed similar success.
Because of the success of that experiment, senior leadership has now decided to elevate this concept to the next level. This fiscal year, we’ll be focusing on five disease states: congestive heart failure, hypertension, diabetes, COPD and substance use disorder. All nine of the service lines and the essential services will be expected to participate in care standardization around these five disease states. Service lines may be accountable for steering the process—for example, cardiology will steer the heart failure process—but every service line is expected to participate.
The goal is to generate collaborative energy between the different components in the organization and create a clinical-pathway-on-steroids that will not just ensure guidelines and standards are respected, but also that collaboration will help us do a more effective job in transitioning care to the ambulatory setting, getting ahead of those disease exacerbations that lead to hospitalizations. Ultimately, we believe that this process will help us achieve the nirvana of true population healthcare.
VALENTINE: Dr. Deering, as the HRS president, you’re looking at atrial fibrillation and ablation and the variability there. We don’t have electrophysiologists in every corner of the country, so this becomes a bigger problem. Can we develop solutions for general cardiologists who are managing atrial fibrillation?
DEERING: That’s the most important question for driving this forward. We need to use the guidelines to inform us, but then put teams together and develop an approach that fits each institution. And we have to have our societies working together. For example, today we are at 60 to 70 percent anticoagulation for indicated atrial fibrillation patients across the globe. The Veterans Administration and other groups have carried that to 92 percent by putting in place pathways that are commonly driven by order sets and engage the clinical team. Societies need to transform the guidelines into pathway-driven clinical tools. The exact mechanisms will vary from institution to institution. Ultimately, we need to throw down the gauntlet and push for high standards and levels of success. This will require a team effort across the specialties. Everybody has to buy into it.
VALENTINE: It is much easier in service lines with large numbers of employed physicians. What about when you have three- and four-person practices working for your hospital?
SCHROYER: The key is in the communication—making sure you get all of the appropriate players in the room and you have discussions. We’ve used the dyad approach—in our case, our cardiology medical director and the service line administrator. You go over the data, look at the variations and the opportunities. You make sure to get everybody’s input. And only then do you come up with a group decision.
Now, not everybody will agree to everything, but you go with the vast majority. Not 100 percent, but 80 or 90 percent. If you’ve made sure everybody had a chance to be part of the solution, almost everyone will go along with it. You might have one or two stragglers, in which case you keep going back to them and showing what the variation did in regard to the quality, or even to the costs. Eventually, they usually will come on board.
AIM TO BECOME A HIGH-RELIABILITY ORGANIZATION
VALENTINE: We hear a lot of talk today about high-reliability organizations, or HROs. Some cardiologists might say, “That’s a C-suite term; how does it apply to me?” Is the HRO idea valid? How do you introduce the idea to cardiologists?
SCHROYER: We’ve gone to our cardiologists with examples of what can happen, especially with safety issues, when you add variances into the mix of patient care. By doing that we’re able to show them why we want to do HRO techniques. Now that we’ve educated our physicians about HROs, they are actually coming to us when they see variations with our staff, so that we can fix it. It is starting to become a partnership. But it does take a while to happen.
GARRATT: About six months after I was hired at Christiana Care, my service line needed a director for safety events—someone who could help manage unexpected adverse events but also help steer quality and safety programs in the right direction.
It’s always useful to have somebody with clinical acumen who can understand the nuances of patient variation and the impact on events. But I went in a different direction in an effort to embed HRO principles into my service line. I hired an HRO expert—an engineer who had worked in a local nuclear reactor facility for several years and was looking for a different challenge. She was with us for about 18 months. I learned a lot, and our safety machinery benefi ted enormously. I don’t know that you have to hire a nuclear engineer but, if you’re serious about embracing HRO principles, you need people in your space who are real content experts, not necessarily clinicians.
BIGA: We’ve established that to achieve high reliability, we need to use guidelines, order sets and pathways. But what about the electronic health record? How are you using your EHR to move toward becoming an HRO?
SCHROYER: For our EHR to help us with this, we need systems that talk and interface with each other, are user friendly and make it easy to input data and information. If you don’t have that, you’re going to be behind with decreasing variability and in improving quality. A lot of today’s EHRs can help us build reports that will give us the data we need and help us track variability easily. But again, if the systems don’t talk to each other, it becomes inefficient and we have to build those reports for each set of data and then manually put it all together.
ROSE: Our tools need to get better. We’ve molded our hand to fit the tool, rather than our tool to fit the hand. We’ve even had to change the way we think and express ourselves based on the limitations of the EHR. So, let’s accept that we’re in need of the next generation of tools.
In the meantime, we have teams of providers taking care of patients, so we have to relay information in simple, common terms. The only way to do this is to standardize how we’re going to communicate. I may like my notes arranged a certain way and you might like yours a different way, but we need to agree on one approach because we need to transfer information with as little friction as possible. There are opportunities, even with the limitations of the tools we have, to improve communications and create standard fields around different conditions. There is more we can get out of the EHR than perhaps we’ve tapped into so far.
BIGA: EHR interoperability will be critical for reducing unnecessary variations in care, specifically in the postacute period. Somehow, we need to get data to our providers more easily while keeping the patient in the middle of everything we’re doing and not duplicating care that was done in the ER, at our hospital across town or even by our colleagues in multispecialty groups. We need answers to the EHR challenge because the EHR needs to be in the center of any discussion about reducing variation in care.
CARDIOVASCULAR SOCIETIES CAN HELP
VALENTINE: What role should the societies play? How can we go from supplying our members with information and data to providing them with partnerships and tools that will help them solve problems?
DEERING: We’ve done a great job with providing education about new and developing technologies and creating guidelines. Where we have fallen short is in carrying it to the next level of preventing unnecessary variation.
There are a number of ways that we can—and we should—do more in that direction. We need to spend more time addressing these issues, such as in our educational sessions. We shouldn’t just talk about the latest scientific studies. Let’s also have presentations that focus on quality outcomes and variation reduction. We also need to have more publications in our journals on these issues.
And we need to train the individuals who will lead our societies and our institutions in this culture and this approach. Could we develop a leadership program across all of the societies and train young, interested individuals first to be champions locally and then to become leaders of, and across, the societies?
ROSE: The societies also can play a role in elevating the importance of the dyad relationship in the architecture and delivery of care. The societies have identified what could be done and what is effective, but we haven’t had the conversations to the same degree on the structure, cost or efficiency of care—the so-called business side of care.
The other aspect that the societies have been engaged in is registries. We talked about benchmarking, which is helpful, but we also need to recognize that when we are putting patients in registries we begin to generate practice-based evidence. We all subscribe to the importance of evidence-based practice, but in reality our evidence base is not as robust as we would like. We literally could (and should) extend this by learning from every patient, but the only way to begin to do that is through registries. The societies have played a role here, but this could be amplified even further.
GARRATT: SCAI has done a nice job on the education part and tried to provide clinical decision aids that can be used inside and outside of the cath lab environment to help reduce practice variation. But I’m struck by how often adverse clinical events have their root in a communication failure, by how often dyad leadership runs into bumps and barriers based on communication failures and by how often colleagues have differences of opinion about clinical care or practice management decisions that often reach unnecessary heights because they don’t communicate effectively.
Tom Lee, now chief medical officer of Press Ganey, demonstrated that, from a patient’s perspective, if it appears that care is being coordinated and there is good communication, almost nothing else matters. Really, truly, if you want to improve your Press Ganey scores, you need to focus on the overt display of coordinated care to the patient and their family and on good communication. If you do those two things, everything else is not nearly as critical to the patient. If those lessons are true for patients, I tend to believe that they’re also true for the apparatus that cares for patients and their families. We need to focus more in that area.
INVEST IN METRICS TO UNDERSTAND BOTH QUALITY & COST
BIGA: What metrics do you use in your service line, and what would you recommend to others, including independent practices?
GARRATT: We use a variety of standing metrics meant to tell us how we’re doing. We organize them into categories. First is our journey toward zero harm. These are standard metrics I suspect everyone follows—hospital-acquired infections, falls and the like. Those data are reviewed in my service line on every nursing floor once a month. Leadership meets with nursing, and we go through the numbers carefully. We look for patterns and trends, and try to sort out how to get ahead of any movement we don’t like.
There also are metrics for organizational vitality, such as our cost-containment exercises, efforts to reduce readmissions, length of stay assessments and so forth. We use the same process to review those and ensure we’re moving in the right direction.
The third category is patient experience. We take the Press Ganey scores incredibly seriously. In the three years I’ve been with Christiana Care Health System, we have launched many programs in direct response to post-hospital surveys of patient experience.
ROSE: Along similar lines, we have service line metrics that we look at on a monthly basis, such as O/E ratios for mortality, readmissions and length of stay. On an individual basis, we look at individual patient satisfaction. On a collective basis, we monitor practice satisfaction in our different locations.
We also have a process within the service line to look at specific metrics germane for each discipline. For example, we have an interventionalist scorecard that looks at a variety of different cath-lab-related metrics, such as complication rates and radial access use.
DEERING: Our approach is similar. We have our quality metrics, which are largely registry and other publicly reported considerations. We certainly look at O/E ratios. We look at patterns of success, complications and patient satisfaction. And we create broad-based pathways metrics in the service line.
Typically, we agree up front that our metrics will have a quality consideration, a fiscal consideration and an operational consideration. We get the entire administrative clinical team to buy into that as an annual goal, which we try to improve every year. We look at the results monthly or quarterly, depending on how relevant the data are and where we are both individually and collectively.
We have full transparency at our meetings. Every doctor’s data are provided. We have frank, honest discussion, not to fi nd fault with someone, but to make everybody better. I’ve been pleased with how our doctors, when seeing the data, have wanted to learn from their colleagues and move in the right direction. We also do transparency across our entire hospital system because we have multiple systems. We look at it that way—we can bring each other up to a higher standard.
BIGA: We look at similar data, but we’ve found it’s important that we differentiate. By that, I mean we look at cost data and quality data.
In addition to what others have mentioned, we’ve added the excess-day report, trying to look at that full continuum as an adjunct, not just the readmission. That will be very important as we continue to look toward the reduction in variation in quality.
From the cost angle, we’re trying to look at costs broken down into the five categories: imaging, labs, pharmacy, length of stay and supplies. All of us probably are extremely challenged with our cost accounting areas while having a better grasp of our quality. Does anyone have ideas, or experience with, becoming a highly reliable organization as it relates to cost data?
SCHROYER: We’re also tracking everything you mentioned but, with regard to cost, you’re absolutely right that everybody’s cost accounting system is less than desirable. We’re all kind of struggling.
We have found that we can tackle cost variations with granular reports. Just showing the number of times certain things are entered per case and then looking at those data for each physician gives us information that’s more helpful than looking at total costs. We run total costs as well, but it doesn’t show a simple story. If you can pull out the DRG data per physician, you’ll be able to see the particular imaging studies, lab tests, everything that has been ordered, which will get you to the variation data you’re looking for.
ROSE: We look at it two ways. First is shifting the cost curve, which is about agreeing to standard approaches with respect to products and so forth, which allows us to deliver at a lower unit price. That takes buy-in and conversation, but once you’ve done it, you have it as a repeated advantage.
The other is to narrow the cost curve, which is where we strive to limit practice variation with care pathways. This work is much harder because it has to happen every day without backsliding to old habits.
VALENTINE: At Centra Health, we’ve been able to use metrics and scorecards that allow our physicians to see lengths of stay, the number of stents and catheters per case, the length and type of ablation, the devices used and so on. As a result, our physicians are able to see opportunities for improvement, or when they’re an outlier among the others in the metrics.
We’re all under great pressure to bend the cost curve. The pressure is not only from administrators, but from payers. We have been helped by showing leadership—particularly in dyad relationships— and by using metrics and communicating well.
BIGA: How well do you think physicians will take to being asked to reduce, for example, imaging? Perhaps they are doing two or three echocardiograms within a single hospital stay when the pathway calls for one. How do you approach that with your physicians so that you can start to change that process?
ROSE: Again, that comes back to the conversations within the service line about creating pathways around those standard diagnoses where we can agree on some common approaches. And I think that’s where we’re able to engineer out what we would consider to be low-value care—those services that don’t actually serve to improve the health of the patient.
GARRATT: This is a place where the EHR can help quite a bit, because once you’ve agreed on a standard of care for a condition, you have the opportunity to bake in soft or hard stops on ordering. I’ve seen that done elsewhere for multiple echo-cardiograms being ordered during a given hospitalization. If there was good reason for the echo to be done, it was easy to get past the barrier, but it was just meant to make the physician pause long enough to create awareness that current echo data were available. Just push this button, and we’ll show you the report. That was quite useful in helping blunt that overutilization issue.
THINK LIKE A LEADER
VALENTINE: How have each of you, as leaders, achieved buy-in with your colleagues on standardizing care and reducing variability?
SCHROYER: The success I’ve had over many years is having good dialogue, good communication and selling the data and the outcome. Showing that, if you do this, this has been the standard outcome. Convincing them to try it and then take a look at the results. Most of the time you can get them to do that, or at least to investigate or talk to their colleagues about it.
DEERING: It’s a hackneyed expression, but it’s very true that culture trumps strategy. Culture also trumps operation. We’re working hard to build a culture where everybody understands that the world is changing; that everybody has to get in the game because healthcare costs rising out of proportion to other components of the economy cannot go on; and that, if we don’t take charge, we’re going be told what to do. We’re providing data to individuals and at the collective level to engage those who have more variation without better outcomes in terms of any metric—whether it be hospitalization, mortality, success or complications—to work together to narrow that variation.
We focus on culture, communication, buying into the program and sharing the data. We have had to ask some people to leave because they didn’t fit. Although that’s hard, it’s important.
GARRATT: Tactically, I can think of two important moves. First, show them the money, and by that I mean two things. One, don’t just claim that there’s a benefit in using a clinical pathway. Show your team the evidence that what you’re saying is true. If you have a standing cardiovascular meeting, use that opportunity to show them the evidence that conforming to a given pathway is going to be best—not just for the hospital, not just for them, but for the patients. Two, be creative in how you gainshare the savings. If you have an employed physician group, you can bake in incentives to reward doctors financially. For independent providers, overtly tie savings to new equipment or services, or the provision of something that a physician wants. Even if it’s just a new coffeepot in the doctors’ lounge. Look for ways to link the cost savings that you’re aiming to achieve with your ability to provide the things they want.
The second move is remembering Abraham Lincoln’s famous saw about the best way to destroy an enemy is to make him your friend. In this context, that means finding physician champions who can help lead the charge on behalf of hospital and service line leadership. In my experience, that has been especially important with regard to nonemployed independent providers. Find opportunities to put independent physicians into leadership positions in your service line so that they can have a clear line of sight with you around these objectives and the rationale behind them. They also can serve as a focal point that’s separate from your employed physician group to help you carry the water on getting goals achieved.
ROSE: I totally agree that you need a guiding coalition. One person or dyad can’t lead this. We need to have other champions whom we’ve persuaded on the merit of this approach. Next, we need to reward those things that are valuable to the organization using whatever mechanisms are available, such as employment contracts or other types of arrangements. There must be sincerity from the organization to show that these efforts are of value.
Also, when it comes to how we approach the work, we expressly say to our providers that these are not cookbook approaches; they are playbooks. There’s a big difference. What we’re doing is constraining the limitless options to a narrower array of options. We find that this turn of phrase is helpful. If we can put all of those things together, we’ve got a fighting chance at making meaningful change.