Cardiology has embraced AI more than most other specialties
Artificial intelligence (AI) algorithms are being used more and more by cardiologists and other cardiovascular professionals. In fact, of the more than 500 clinical AI algorithms cleared by the U.S. Food and Drug Administration (FDA), cardiology has more than all but one other specialty: radiology has more than 400, and cardiology has more than 60.
Those numbers continue to grow, suggesting that this is just the beginning for cardiology's relationship with this evolving technology.
Beyond the clinical, patient-facing AI algorithms the FDA reviews, there are hundreds more non-clinical algorithms now embedded into back-end health IT systems to speed workflow, improve efficiency, complete time-consuming tasks, analyze data and more.
Here is the breakdown for the number of FDA-cleared algorithms across specialties as of the FDA's last update in January 2023.
• Radiology 396
• Cardiology 58
• Hematology 14
• Neurology 10
• Clinical chemistry 7
• Ophthalmic 7
• Gastroenterology and urology 5
• General and plastic surgery 5
• Pathology 4
• Microbiology 4
• Anesthesiology 4
• General Hospital 3
• Orthopedic 1
• Dental 1
See the complete list of FDA-cleared algorithms here
Additionally, the American College of Radiology (ACR) also maintains a frequently updated database of medical imaging AI FDA approvals. According the the ACR database, and additional 35 medical imaging AI algorithms were cleared between January and March 30, 2023. This included 8 new cardiac related algorithms, bringing the total for cardiology to 66. Radiology algorithms overall are now at 431.
The first AI algorithm was cleared by the FDA in 1995, and fewer than 50 algorithms were approved over the next 18 years. However, the numbers have increased rapidly in the past decade, and more than half of algorithms on the U.S. market were cleared between 2019 to 2022––more than 300 apps in just four years. Last October, the FDA approved 178 new AI and machine learning (ML) systems. That number is expected to grow rapidly into the future, the FDA has said.
Getting AI buy-in from cardiologists
Ami Bhatt, MD, the American College of Cardiology (ACC) chief innovation officer and adult congenital heart disease cardiologist at Mass General Hospital, said artificial intelligence really needs to be renamed "collaborative intelligence," because it is really a collaboration between a human doctor and the machine to leverage the best abilities both have to offer to improve patient care and efficiencies in healthcare. The ACC has been a big advocate for bringing more cardiology AI to the market to help augment physicians amid a growing shortage of cardiologists in the U.S.
"It's simply that the human eye can't necessarily take all of that data and process it the way a computer can. So we are not saying we are replacing humans with computers, we are trying to allow clinicians to work at the top of their license and to given them some guidance as to what may be a good direction to go in. And there are times when our clinical acumen will supersede what a computer may suggest, and that is OK and that needs to happen, because then we reteach that computer how to learn," Bhatt explained.
Bhatt also emphasized that this does not mean every physician has to be an expert when it comes to AI.
"[Physicians just] need to understand there is some AI here with computational aspects, and here is what it is meant to do. Any beyond that, they just need to use their clinical acumen," she said.
Bhatt and others have also noted that AI needs to be seamlessly integrated into workflow, just like medical devices or reporting software to make it usable by clinicians.
What cardiologists need to know about AI
"We really need to upscale cardiologists' understanding of this technology. We live in a digital world and medicine tends to be fairly conservative, but I think people are recognizing AI is here to stay and we have to embrace it. In the clinical community, we need to be at the forefront," explained Ed Nicol, MD, consultant cardiologist and honorary senior clinical lecturer with Kings College London, and president-elect of the Society of Cardiovascular Computed Tomography (SCCT).
The academic discussions on AI and its future applications are largely over. What is now being discussed are actual FDA-cleared products sold on the market and in clinical use.
Making this more real is the fact that the first cardiology AI algorithm is now included in practice guidelines in both Europe and the United States. The ACC/AHA 2021 Chest Pain Guidelines include the recommended use of AI-driven fractional flow reserve hemodynamic flow measurements derived from noninvasive CT imaging (FFR-CT).
"If you had said to me 15 years ago we were going to have some sort of computational fluid dynamics tool in the U.S. chest pain guidelines, you would have been laughed at. Everyone would have said you were crazy. But that is the reality, we see FFR-CT in the international guidelines, based on evidence. That will be the first, I suspect, of many," Nicol said.
He said the biggest thing cardiologists need to understand is how the AI they are evaluating or using works. This way they can understand if there are issues in the AI-generated data and how they should validate it.
"We the clinicians really need to own this," Nicol explained. "And you can really only own this and challenge it if you understand it and the strengths and weaknesses of AI. We are not trying to change the whole radiology/cardiology community into programmers, but they need to understand how those programs work, even if they do not understand all the strings of computer code."
"One of the things I am amazed about is the rapid progression of non-invasive imaging and using artificial intelligence to try and standardize analysis," explained Juan Granada, MD, president and CEO of the Cardiovascular Research Foundation (CRF), when describing key technology trends he sees in cardiology.
AI in cardiac imaging enables faster exam reads by automating quantification and making measurements more consistent, eliminating the usual variability between radiologists or cardiologists. Granada believes AI will soon play a big part in cardiac care in all of its the subspeciality areas, including interventional cardiology.
While there are FDA-cleared AI algorithms to automatically assess ECG data and wearable heart monitor data, most of the cardiac AI has been concentrated in imaging. In addition, many of the radiology-cleared algorithms are actually specifically for cardiovascular, peripheral vascular and neurovascular imaging. These include uses in CT, MRI, nuclear imaging and cardiac ultrasound.
AI in echocardiography
"AI is coming along in many areas of echocardiography. It is just exploding and it is very exciting," explained echocardiography expert Patricia A. Pellikka, MD. She is the editor-in-chief of Journal of the American Society of Echocardiography, director of the Mayo Clinic Ultrasound Research Center and a consultant for Mayo Clinic department of cardiovascular medicine. "One of the areas is the use of AI too help improve ultrasound acquisition of images by teaching inexperienced users how to get the image. Another area is applying AI to the data that is already acquired to remeasure things, or to apply AI to all the measurements that have already been obtained to detect disease."
In her research at Mayo, Pellikka has been involved with the development of AI that looks at the ultrasound images to directly detect disease. The algorithms can pick out radiomic signatures of disease in the image that may not be evident to the human eye.
"I think the potential there is enormous," Pellikka said.
Over the past few years there has been a big increase in the use of point-of-care ultrasound (POCUS) systems in a variety of settings, including clinics, physician offices, emergency departments and ICUs. These echos are being performed by much less experienced sonographers than those in hospital echo labs. A couple AI vendors have developed FDA-cleared algorithms to show POCUS users how to move their probe into the correct position and walk them through how to acquire each of the standard echo views. The AI also tells the operator when they are in the correct position and judges the quality of the images they are acquiring. Many echo experts say this can significantly improve exam diagnostic quality, leading to fewer repeat exams, faster and better diagnosis of patients.
"This will extend the reach of cardiovascular ultrasound to places and times when there isn't an experienced cardiac sonographer available to do the imaging. I think the potential for this is extremely exciting," Pellikka explained.
AI is also being used to speed up patient assessments by automating echo strain, ejection fractions and other measurements. Pellikka said several vendors have now developed FDA-cleared algorithms in these areas. This automation can eliminate the need for a sonographer to perform manual contouring of the ventricles, or manually using calipers to take various measurements. She said the sonographer can still edit these AI-generated contours if they feel they are incorrect. Overall, she said this results in a much faster exam or post-processing of the exam, enabling more patient throughput.
Importantly, Pellikka and other echo experts say this type of AI automation also reduces the variability in measurements between different sonographers. AI automatically picks the same landmark locations to perform measurements, helping deliver more consistency. This is especially important when monitoring patients over time.
"I think this is just the tip of the iceberg and I think we will be automating many other measurements as well, such as automatic assessment of valvular heart disease. All of this is going to increase the standardization of echocardiography and make it so the communication between one center doing an echo and another is more standardized than it is today," Pellikka said.
AI in cardiac CT
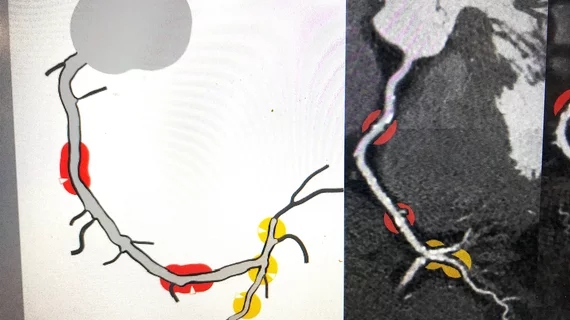
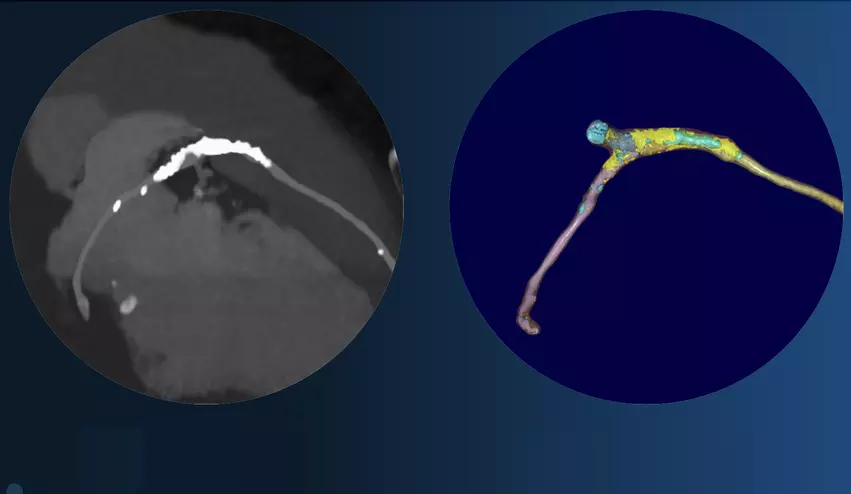
AI that automates CT calcium scoring and measurements has been around for a few years now, but the big advancement in cardiac CT has been new FDA-cleared algorithms to automatically analyze soft plaques in the coronaries, including looking for vulnerable plaques. This can be used to better assess risk and to track preventive treatments before atherosclerosis progresses to cause heart attacks. Two vendors now have FDA clearance for this technology. Read more.
"What a lot of these AI companies are now saying is that we can use this technology to go back along the clinical pathway, so we are not waiting for people to get ischemia," Nicol said. "This can move us away from primary and secondary prevention to just continuous prevention. So we can stop people from having angina, acute coronary syndrome or a heart attack. I think we do now have the tools and technology to allow us to do that, but I think the really interesting thing will be how you embed these novel technologies into clinical practice."
In discussions with some of the AI vendors that are focused on CT plaque assessment, the question was raised as to why a cardiologist would need AI to assess plaque burden numbers to two decimal places. Nicol has since realized AI is opening many new possibilities no one ever thought of before.
"Originally I thought, that makes no sense to me, but that was before speaking with the vendors to understand the context of why theses companies are developing these tools," Nicol said. "If you are going to follow people over time, if you are going to use CT as the test to demonstrate if your statin or PCSK9 is working, that makes sense. The patient might be a non-responder to the medication, or they might need a second medication. That's when those kinds of precise quantifications make sense."
He said AI can now enable cardiologists to actively prevent disease progression in patients, rather than just being reactionary to acute coronary episodes. While manually performing soft plaque measurements can be done, no one will take the large time needed to actually do it because reimbursements would never cover the expense of time.
"Soft plaque evaluation is something we have been talking about for nearly two decades, but the limitations always have been how to overcome the large amount of post-processing times," explained 2021-22 SCCT President Eric Williamson, MD, MSCCT, associate chair for radiology informatics at Mayo Clinic Rochester, supervisor of the radiology artificial intelligence program and professor of radiology at Mayo Clinic. "Previously, it was very time and labor intensive. But, with the advent of AI and machine learning, this process can be automated."
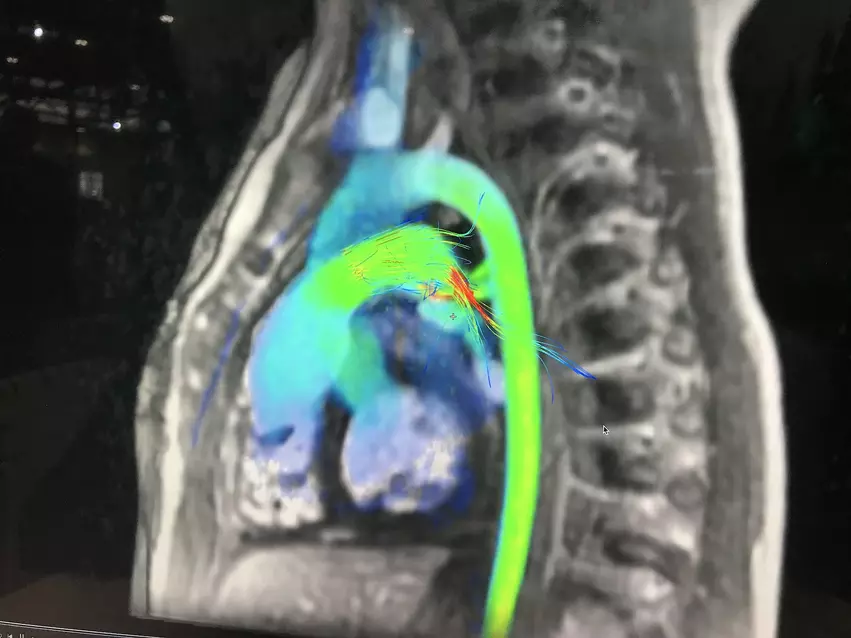
AI in cardiac MRI
A few MRI vendors have integrated AI into their systems to greatly simplify workflow and speed exam and post-processing times. One example is a new AI workflow recently adopted at Brigham and Women's Hospital. The AI picks the MRI views and enables the acquisition with just one click. The AI also provides all the measurements and quantification automatically.
"What that has done for us is it impacted many important areas," explained Marcelo DiCarli, MD, chief, division of nuclear medicine and molecular imaging, executive director for the cardiovascular imaging program, Brigham and Women's Hospital. "Number one, it shortened the examinations. It is good for patients because they don't need to spend as much time in the magnet, but it is also better for throughput because we can accommodate more patients on any given day. Number two, it has increased the quality of what we do, because it is less dependent on the expertise of the technologists who are pressing the buttons and making decisions. And then on the post-processing, it has simplified our lives. What used to be a very time-consuming process is now just a click away. For me, that is very impactful."
AI in nuclear cardiology
"One of the Achilles heels of SPECT imaging has been attenuation artifacts, and now we have a deep-learning based approached to attenuation correction that does not require extra equipment," DiCarli added. He said commercialized AI can be used to perform virtual attenuation correction on older SPECT scanners without the need to upgrade to newer, expensive imaging systems.
In PET, AI can independently assess coronary calcium using the non-gated, attenuation correction CT scan on the PET-CT systems.
Cardiac imaging AI on the horizon will soon include algorithms for opportunistic, automated CT calcium scoring on chest CTs that are being done for other purposes. Radiomics is another area that will also likely see rapid growth in the coming years, where AI scans image data for very complex and subtle patterns that can show a predisposition to some diseases, offer new types of risk assessments, and show worsening disease progression long before the patient is symptomatic.