Cardiac CT now in the spotlight thanks to chest pain guidelines
Advocates for cardiac computed tomography (CT) have been saying for the past decade that CT offers many advantages for the evaluation of chest pain. This was officially recognized last October with the release of the American College of Cardiology (ACC) and American Heart Association (AHA) 2021 Chest Pain Evaluation Guidelines. In the guidelines, cardiac CT was elevated to a top 1A, front-line test indication.
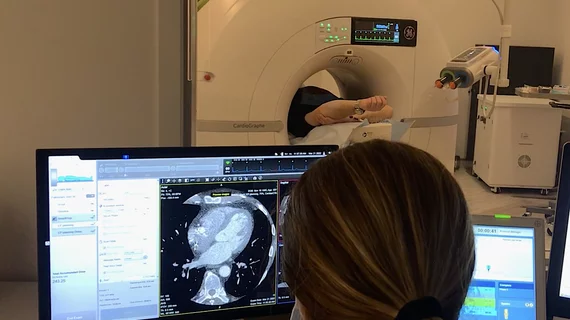
While some hospitals were already using CT in emergency departments (ED) for triage, a large number of new centers are now looking to begin more comprehensive cardiac CT angiography (CTA) programs. The guidelines focused on hospitals on the fence about creating CTA programs, and it is very clear interest is rising rapidly.
Vendors with CTA technologies at the 2022 ACC meeting in April said they were swamped with serious conversations with physicians and cardiology department administrators. The Society of Cardiovascular Computed Tomography (SCCT) broke all previous attendance records at its 2022 meeting in July, despite attendance being lower at most in-person medical conferences as COVID-19 restrictions continue to wane. Vendors exhibiting at the SCCT meeting also said they had much higher engagement with attendees compared to previous years. A CTA accreditation company exhibiting at SCCT also said they have seen a massive increase in cardiologists and radiologists looking to get certified in CTA since the guidelines were released.
Eric Williamson, MD, MSCCT, 2021-22 SCCT president and professor of radiology at Mayo Clinic, said there has been a 60% increase in CCTA exams at Mayo over the past year or so. He said this was partly fueled by COVID-19, where a CT scan that is almost contactless was seen as an advantage over other tests with closer or prolonged contact with patients. He said the change in guidelines and a movement toward multi-specialty care teams also helped fuel this rise.
He said there has been close coordination between emergency department (ED) physicians, cardiologists and radiologists at many hospitals in recent years to take a care-team approach to address chest pain presentations in the ED.
"The guidelines give a new 1A indication for cardiac CT for the evaluation of stable and acute chest pain," Williamson said. "We believe in our community this is long overdue. But it is nice to see the broader medical community of medical care acknowledging and understanding the strengths of this technology."
Many key academic cardiology centers have been using CTA for years as a first-line test. Massachusetts General Hospital has been using CT angiography as a primary test to evaluate chest pain since 2014, explained SCCT President Brian Ghoshhajra, MD, MBA, division chief, cardiovascular imaging, at Mass General, and associate professor of radiology, Harvard Medical School.
"It's a disruptive technology," Ghoshhajra said. "It can certainly obliviate the need for invasive tests. What is well codified in the new guidelines is that there are many first-line tests for different types of patients, and sometimes there are choices. We strongly feel CT is often a first-line test, more so than what prior guidelines had reflected. I would say the first-line indication is highly appropriate in a large and ever growing number of patients."
Details of the 2021 chest pain guidelines
"There are many tests with a Class 1A recommendation, and cardiac CT is not always going to be the right test for everyone," explained Ron Blankstein, MD, MSCCT, associate director, cardiovascular imaging program, director, cardiac computed tomography, Brigham and Women's Hospital, and professor of medicine, Harvard Medical School. He also was a co-author on the 2021 Chest Pain Guidelines.
"In particular, coronary CTA would be useful in patients who do not have known coronary artery disease (CAD) who have an intermediate to high pre-test probability of having obstructive disease," Blankstein explained
While not always the first test choice, he said these factors favor use of coronary CTA (CCTA):
• Younger patients who are not on preventive therapies.
• Individuals where the objective of testing is to identify non-obstructive or obstructive coronary artery disease.
• This includes scanning patients where there was a previously inconclusive stress test.
The guidelines also put a new emphasis on non-obstructive coronary artery disease.
"This guideline is the first time ever that non-obstructive CAD is now classified as coronary disease, and there is a Class 1 to optimize preventive therapies for those patients," Blankstein said. "Coronary CT gives us an opportunity to identify non-obstructive disease, which we might not identify on other types of stress test imaging."
CTA also can be used as a gatekeeper to decide which patients get sent for diagnostic angiograms in the cath lab.
"In the new guidelines, particularly for patients with stable chest pain, there is no longer a category of patients who should go directly to invasive angiography," he said. "The use of imaging in general, including coronary CTA, should always be done, and this is why those intermediate- and high-risk patients are both grouped as a single group when we are deciding whether to do further testing."
The guidelines state CCTA has a 1A recommendation for anatomical imaging for intermediate-risk patients with acute chest pain and no known CAD eligible for diagnostic testing after a negative or inconclusive evaluation for ACS, CCTA is useful for exclusion of atherosclerotic plaque and obstructive CAD.[1-11]
CCTA had a 2A recommendation for intermediate-risk patients with acute chest pain with evidence of previous mildly abnormal stress test results (within one year), CCTA is reasonable for diagnosing obstructive CAD.[12,13]
The guidelines also recommended the use of non-invasive fractional flow reserve-CT (FFR-CT) in select patients. More information on this technology is in the subsections below.
Large amount of clinical evidence led to change in guidelines for CCTA
"In the last iteration of the guidelines, cardiac CT got a 2A or 2B, which is a lower indication, but the 1A in these guidelines is the highest level indication that you can get for any type of testing, and that is a byproduct of the evidence," explained Leslee Shaw, PhD, FACC, MASNC, FAHA, FSCCT, clinical scientist and director of The Blavatnik Family Women’s Health Research Institute, Mount Sinai Hospital, New York. She is a former president of both the SCCT and the American Society of Nuclear Cardiology (ASNC), and was a co-author on the 2021 Chest Pain Guidelines.
Many cardiac CT imagers have believed for a decade or more that CCTA should be a first-line imaging modality for chest pain because it offers more information than other modalities, it is noninvasive, and has the potential for faster discharge. But Shaw said CCTA advocates were told they needed to gather large amounts of clinical trial evidence to show the modality has benefits before guidelines committees would recommend it as a front-line imaging modality.
So CT investigators, along with support from the SCCT, sponsored a large number of trials since 2000 to gather that evidence. Collecting this data has been one of the main priorities of SCCT over the past decade.
"I think the recent chest pain guidelines are proof positive of what can happen when a field dedicates itself to providing better evidence to guide clinical care," Shaw explained. "I think CT really has a tremendous amount of evidence, and in the guidelines we included 19 randomized trials, which is a lot."
Getting started in cardiac CT
With the elevation of CCTA in the guidelines, Blankstein said there has been a lot more interest since late last fall.
"We are seeing increased interest in coronary CTA, and frankly we say that even before the guidelines, but the guidelines will likely fuel that even more," Blankstein said. "I think there are a lot of hospitals that are looking to invest more in coronary CT, and it does take a lot of investment."
He said hospitals making the investment need to ensure that they have the right equipment, and the right people in terms or radiologists or cardiologists who can read the studies.
In response to the wave of interest, SCCT is building a new website called the SCCT Starter Kit. It will provide materials, resources and advice to centers looking to create or expand their cardiac CT programs.
"If you do have a 64-slice scanner, that is the minimum price of entry into cardiac CT," Ghoshhajra said
He said it's not just the number of slices, but the speed of the scanner, the type of iterative reconstruction the system uses to create images, field of view and the gantry rotation speed. Technologists also need to be proficient in CCTA, able to setting up patients with ECG leads attached to the ECG triggering system on the CT scanner, understand the imaging protocols, and be able to set up and coordinate the contrast injection during the scan.
"Coronary CT angiography is a highly technically demanding sub-speciality exam to both perform and interpret," Ghoshhajra said. "The fact remains that there are not a lot of interpretive skill for this, and the scans don't yet read themselves. It does require expertise to read and acquire these scans."
He said most EDs now have 64-slice and greater CT scanners that are cardiac capable. Creating a cardiac CT program does require expertise, and staff may require additional training. He said there are training resources available through SCCT for technologists, cardiologists and radiologists.
Read and hear more in the VIDEO: Cardiac CT training requirements for radiologists and technologists — Interview with Brian Ghoshhajra MD
Elevation of CTA indication offers a new business model for cardiology
It has been predicted for years by SCCT experts that in the future, cardiac CT could be used in an outpatient setting as a standard-of-care to evaluate non-acute chest pain and offer more detailed coronary risk assessments by looking at soft plaques and calcium scoring. That prediction is now becoming a reality in the wake of the 2021 chest pain guidelines.
One of the first outpatient dedicated cardiac CT programs was started in the fall of 2021 by Duly Health and Care, in the Chicago suburb of Lisle. They use the dedicated cardiac CT scanner for stable patient chest pain evaluations and for structural heart evaluations and transcatheter procedural preplanning.
"We have been finding that as the technology of CT angiography has improved more and more over the years, we also are finding we are leaning on it more for diagnosis of coronary artery disease and chest pain syndromes in patients. We also found we were sending patients to the hospital environments to obtain that imaging, but we have had such a robust volume of cases for our large practice, we started investigating if it made sense to bring CT imaging in-house," explained Evans Pappas, MD, chair of the Duly Department of Cardiology.
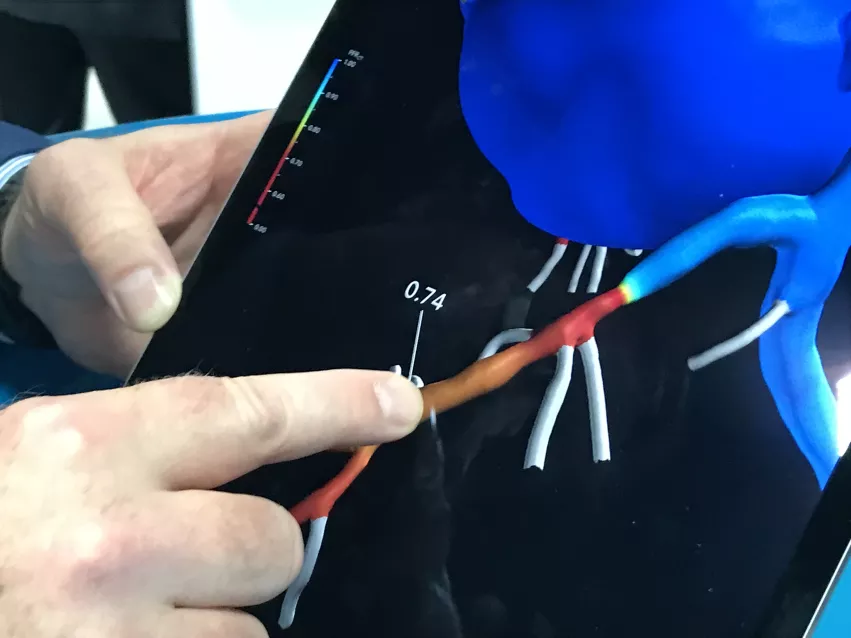
All patients who are scanned and have at least a 30% blockage in a coronary artery are also evaluated with fractional flow reserve CT (FFR-CT), which also was included in the new chest pain guidelines. This offers physiologic information and serves as a non-invasive version of a diagnostic angiogram and invasive pressure wire FFR used to assess the severity of flow limitation by a blockage. This can also help determine if a patient really needs percutaneous coronary intervention (PCI), or if they can be managed with medication.
Cardiovascular Business visited the clinic in March 2022 and produced this VIDEO: Office-based cardiac CT and FFR-CT offer a new business model.
FFR-CT is included in the 2021 chest pain guidelines
Fractional flow reserve-CT was included in the 2021 chest pain guidelines as a 2A recommendation. It was given a level of clinical evidence of B-NR, which means it has moderate quality evidence from one or more, well-designed and executed nonrandomized studies. The guidelines cite six studies.[15-20]
For intermediate-risk patients with acute chest pain and coronary artery stenosis of 40% to 90% in a proximal or middle segment on CCTA, the guidelines state FFR-CT is reasonable for diagnosis of vessel-specific ischemia and to guide decision-making regarding the use of coronary revascularization. From one large clinical registry, the deferral of coronary revascularization with a normal FFR-CT was safe, with no difference in MACE at 90 days.[19]
The guidelines also stated patients with acute chest pain who have coronary artery stenosis from 40% to 90% on CCTA may benefit from measurement of FFR-CT, especially when the stenosis is proximal or mid-coronary artery.[15-20]
Ghoshhajra said FFR-CT is often used when there is an intermediate grade stenosis, and the reader is not sure if it is significant enough for revascularization or not. He said the FFR-CT can show the physiologic consequence of the lesion, which cannot always be determined from anatomical imaging alone.
"And even in the invasive angiography lab, it is not always possible to visually predict the stenosis grading. We have known that for a while through the FAME and the DEFER trials," Ghoshhajra explained. "But what can be done with an invasive flow wire, can be virtually predicted noninvasively with a high level of accuracy using computational fluid dynamics."
Shaw said about half of significant stenosis seen on CT are ischemic and need to be revascularized. The rest may look bad, but are not causing problems for the patient. FFR-CT can help separate out the lesions that are actually an issue and can qualify the amount go severity.
She said there is now a large amount of evidence showing the value and accuracy of FFR-CT, enough that most of the guideline committee members supported its inclusion and elevating its indication. It also offers advantage that a single test can provide both anatomical and physiological assessment.
"With FFR-CT, we have to remember that you don't have to send a patient for another test," Shaw said. "If you are concerned about that stenosis being ischemic, you don't have to stop and re-order another test, send them to stress MRI or stress nuclear, you can send the existing CT for evaluation in one test so we are cognizant of the patient's time. So there are a lot of distinct advantages with FFR-CT. It gives you the physiological significance of that specific stenosis, where as the stress imaging modalities are not that specific."
Opposition in CT's new elevated status from competitive nuclear and MRI societies
The chest pain guidelines was a collaborative effort involving not just the AHA and ACC, but including several cardiac imaging societies. All but one of these societies endorsed the guidelines. The American Society of Nuclear Cardiology (ASNC) said they could not endorse it because they felt FFR-CT was given too high of an “inappropriately” large role in evaluating chest pain. ASNC leadership believed multimodality imaging and risk scores were being short changed by this newer technology.[21]
“The lack of balance in the document’s presentation of the science on FFR-CT and its inappropriately prominent endorsement detract from ASNC’s core principle of patient first imaging,” wrote Randall Thompson, MD, ASNC 2021 president, and Dennis Calnon, MD, 2022 ASNC president, wrote in a letter to ASNC members last fall when the guidelines were released. “We believe that the document fails to provide unbiased guidance to healthcare professionals on the optimal evaluation of patients with chest pain.”
They said all stress testing (SPECT MPI, PET MPI, etc.) should not be bundled together and expressed concerns the guidance may promote harmful test substitution policies.
“There are many excellent, evidence-based recommendations in the new guideline. There also are some troubling recommendations and some omissions that, in the end, ASNC cannot support,” Thompson and Calnon stated.
"Our main objection was that FFR-CT is not widely available. It is expensive and there is only one vendor. The guidelines did not include the limitations of FFR-CT, while it including the limitations for every other modality," Thompson explained in an interview with Cardiovascular Business this past spring.
"I was disappointed," Shaw said of ASNC not supporting the endorsement of cardiac CTA. She is a former president of both SCCT and ASNC. "First of all, cardiac CT got everything it deserved in that guideline. What I tell the ASNC community is that I wish they would focus on their own modality and doing better, high quality SPECT and doing more PET imaging to grow the field instead of worrying about another modality."
Shaw explained that CCTA is a different approach than the standard of care for 20 or more years. "Being concerned about a different approach is just sort of short-sighted, and it does not offer their community a lot of what their future is about."
She said FFR-CT is not used very much today because of limited access, as compared to large volumes of nuclear cardiology. "We are not in a situation where FFR-CT is all of a sudden going to overtake nuclear cardiology from a business standpoint.
Shaw said the ASNC stand against supporting the guidelines was short sighted in her opinion because the more the cardiac imaging indications expand, usually everyone benefits from increasing numbers of patients coming in seeking exams. "That is the approach we should all embrace, that the more ischemia testing we do, likely the we will see utilization of nuclear and all other modalities across the field," Shaw explained.
The Society of Cardiac Magnetic Resonance (SCMR) supported the guidelines, but published an overview that states the recommendations of FFR-CT were "premature."[22] The authors said the diagnostic and prognostic utilities of FFR-CT are not as robustly evidenced as any of the stress imaging modalities (stress CMR, SPECT, PET, and stress echocardiography). SCMR authors also said the ischemia imaging modalities were inappropriately compared as a group against anatomical CCTA in the guidelines. Thompson said the article was a good overview of the same reasons ASNC had to opposing the guidelines. Read the article "Society for Cardiovascular Magnetic Resonance perspective on the 2021 AHA/ACC Chest Pain Guidelines."
Here more details in these interviews:
VIDEO: Why the ASNC did not support the 2021 Chest Pain Evaluation Guidelines — Interview with Randall Thompson, MD
VIDEO: Cardiac CT now recommended as a front-line chest pain assessment tool — Interview with Leslee Shaw, PhD
Related SCCT and Cardiac CT Content:
VIDEO: The role of cardiac CT in the 2021 chest pain guidelines — Interview with Ron Blankstein, MD
VIDEO: The new role of cardiac CT under the 2021 chest pain evaluation guidelines — Interview with Eric Williamson, MD
VIDEO: Cardiac CT now recommended as a front-line chest pain assessment tool — Interview with Leslee Shaw, PhD
PHOTO GALLERY: Cardiac CT advances at SCCT 2022
Cardiac CT soft plaque assessment may offer paradigm shift for coronary disease screening
VIDEO: CT imaging to plan coronary interventions — Interview with Jonathon Leipsic, MD
VIDEO: 3 challenges for Society of Cardiovascular Computed Tomography members in 2023
New CAD-RADS 2.0 reporting for coronary CTA offers patient management recommendations
VIDEO: Why plaque composition CT imaging may be the future of cardiology — Interview with Prof. Jeroen Bax
VIDEO: The new role of cardiac CT in chest pain evaluation — Interview with Brian Ghoshhajra, MD
VIDEO: Use of CT to assess coronary plaques — Interview with Leslee Shaw, PhD
VIDEO: Top 6 takeaways from the Society of Cardiovascular CT 2022 meeting — interview with Eric Williamson, MD
VIDEO: New Technologies in Cardiac CT Imaging — Interview with Ron Blankstein, MD
Find more cardiac CT news and video
References: