Electrophysiologists debut new technology that builds interactive cardiac maps out of 12-lead ECGs
The University of California San Diego Health has debuted a new technology that may offer a better way to assess and treat arrhythmias such as atrial fibrillation (AFib).
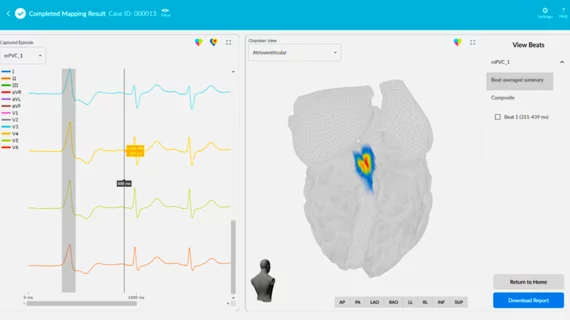
The vMap system is a noninvasive, computational mapping system that produces a 3D, interactive map of arrhythmia hotspots anywhere in the heart. It can pinpoint the source of cardiac rhythm issues in all four chambers of the heart, the septal wall and the outflow tracts. The system creates an electrophysiology (EP) electromap of the heart in minutes using only data from a standard 12-lead electrocardiogram (ECG).
The standard of care for treating AFib is catheter ablation, when specialists burn or freeze specific cardiac tissue responsible for the errant electrical signals causing the abnormal heartbeat. A common issue, however, has been locating these specific areas that need to be treated. Traditional arrhythmia mapping techniques take a lot of time and energy, and physicians are only able to achieve complete success in a limited number of ablation procedures due to the lack of information about arrhythmia source locations. In fact, AFib recurs following catheter ablation in up to 40% of cases.
Mapping the heart prior to the procedure can take more than an hour and is a time consuming part of these procedures. This new technology can create the electoral mapping prior to the procedure, which can aid planning and greatly reduce procedure times.
“My team and I experienced first-hand the limitations of the current standard of care for understanding and treating arrhythmias,” David Krummen, MD, cardiac electrophysiologist at UC San Diego Health and professor of medicine at University of California San Diego School of Medicine, said in a prepared statement.
Krummen co-invented vMap and serves as clinical advisor to the company that developed the technology, Vektor Medical.
“We designed vMap to improve ablation outcomes by rapidly providing arrhythmia source information to the physician," he said. "We want this technology to increase first-pass ablation success, decrease procedural risk, and improve the care of patients with heart rhythm abnormalities.”
vMap received FDA clearance in November 2021. The system converts ECG data into 2D and 3D arrhythmia source maps using data leveraged from millions of arrhythmia simulations performed by technology resources, including the UC San Diego’s San Diego Supercomputer Center.
The results from vMap’s first clinical study will be published later in 2022.