World’s first dual-chamber leadless pacemaker still going strong after 6 months
Abbott’s Aveir DR leadless pacemaker, the world’s very first dual-chamber pacing solution of its kind, is associated with a “reliable” performance after six months, according to new data published in Heart Rhythm.[1]
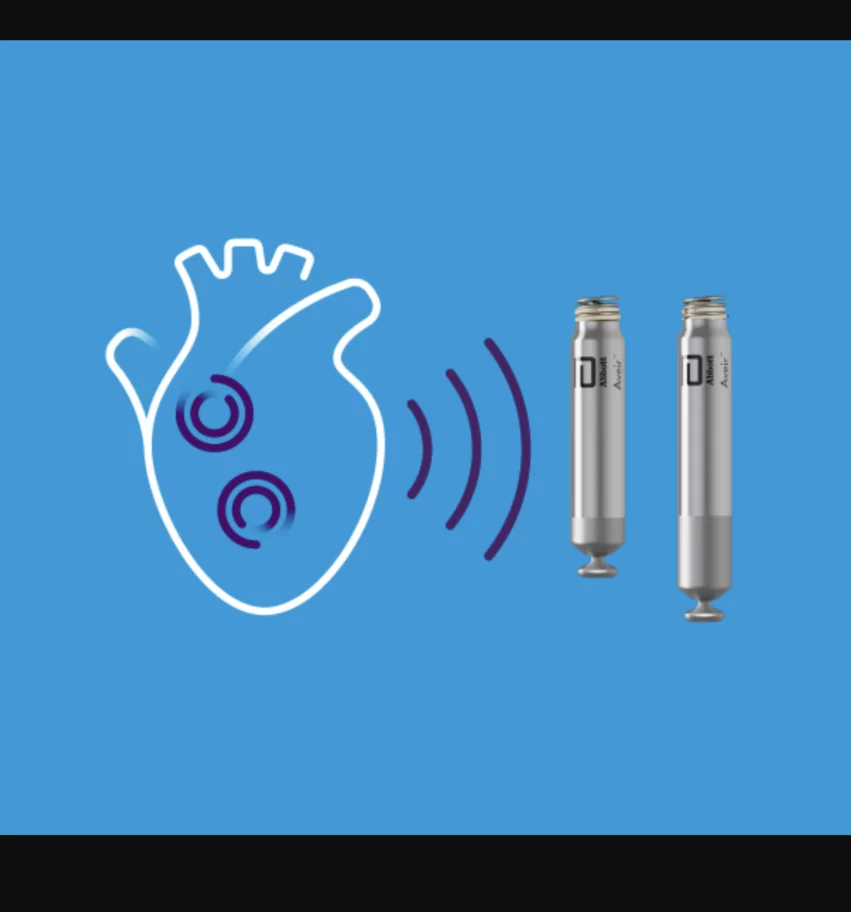
The Aveir DR system includes both an atrial leadless pacemaker (ALP) and a ventricular leadless pacemaker (VLP). The two devices were designed to communicate with one another as needed, helping patients with abnormal heart rhythms receive the care they need at any given time.
The U.S. Food and Drug Administration (FDA) approved the new-look device in July 2023, making leadless pacing available to a much wider patient population. While single-chamber leadless pacing has been around for several years, most bradycardia patients require dual-chamber pacing.
Now, researchers are sharing an updated look at the Aveir DR system’s performance six months after implantation. The group evaluated data from 381 patients treated with the device from February 2022 to March 2023. The mean age was 69.3 years old, and 61.7% were men. The mean left ventricular ejection fraction was 60.1%, 34.6% presented with a history of atrial fibrillation (AFib) and sinus node dysfunction was the primary indication in a clear majority (65.4%) of patients.
In the six months following implant, ALP pacing was delivered in 36.4% of beats and VLP pacing was delivered in 30.6% of beats at a programmed base rate of 55.9 bpm.
For just sinus node dysfunction patients, ALP and VLP pacing were delivered in 45.8% of beats and 18.6% of beats, respectively, at a base rate of 56.9 bpm. For all other patients, meanwhile, ALP and VLP pacing were delivered in 18.7% of beats and 50.4% of beats, respectively, at a base rate of 53.9 bpm. Phrenic nerve stimulation was seen in two patients and resolved by reprogramming pulse amplitude.
In terms of electrical performance, the Aveir DR system was associated with a pacing capture threshold and sensed amplitude measurements that improved significantly from implant to the end of the first month.
While ALP impedances “increased acutely from implant to discharge, and gradually reduced through six months,” VLP impedances “continually reduced from implant until three months, stabilizing thereafter.”
Researchers noted that electrical performance did not seem to be dramatically impacted by exactly where the Aveir DR system was implanted.
“The lack of correlation between pacing or sensing and implant location suggests that targeting a specific anatomical location is not required to achieve stable electrical contact,” wrote first author Gerhard Hindricks, MD, PhD, a cardiologist with the German Heart Institute Berlin, and colleagues. “Thus, implant location selection can be guided by other device performance considerations, such as implant-to-implant communication.”
Hindricks et al. also noted that these patients were clear candidates for the Abbott technology.
“Although simple atrial tracking, rather than pacing, may suffice for some patients, the need for dual-chamber pacing was evident in this study population by the overall atrial pacing burden observed at six months,” they wrote. “As expected, atrial pacing was particularly prevalent in patients with sinus node dysfunction, with pacing delivered by ALPs in 45.8% of beats. However, atrial pacing was also delivered in 18.7% of beats in patients without sinus node dysfunction, for whom diagnosed or undiagnosed secondary indications may also be addressed.”
Overall, researchers concluded, this first-in-human evaluation “demonstrated reliable electrical performance” six months after implant.
It is worth noting that several of this study’s authors receive consulting fees from Abbott. In addition, one co-author is an Abbott employee.
Click here to read the full analysis in Heart Rhythm, an official journal of the Heart Rhythm Society.
![Abbott’s Aveir DR leadless pacemaker, the world’s very first dual-chamber pacing solution of its kind, is associated with a “reliable” performance after six months, according to new data published in Heart Rhythm.[1]](/sites/default/files/styles/top_stories/public/2024-05/screen_shot_2024-05-10_at_11.33.50_am.png.webp?itok=Oy9yMpKh)