Heart surgeons detail world’s first robotic heart procedure of its kind
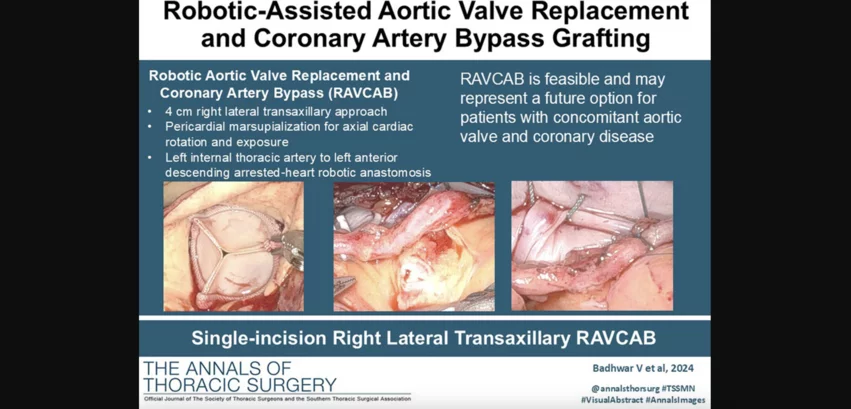
In October 2024, heart surgeons with the WVU Heart and Vascular Institute in Morgantown, West Virginia, performed the world’s first robotic aortic valve replacement and coronary artery bypass (RAVCAB) procedure. Now, the team behind that historic surgery has shared its full story for the first time, publishing an in-depth look at the procedure in The Annals of Thoracic Surgery, an official journal from the Society of Thoracic Surgeons.[1]
“Robotic assisted off-pump minimally invasive direct coronary bypass and totally endoscopic coronary artery bypass (TECAB) have been established as possible left chest approaches to grafting a stenosed left anterior descending (LAD) coronary artery,” wrote first author Vinay Badhwar, MD, executive chair of the WVU Heart and Vascular Institute and chair of WVU’s department of cardiovascular and thoracic surgery, and colleagues. “Robotic aortic valve replacement (RAVR) performed via a 3-cm lateral transaxillary mini-thoracotomy has been established as a method to treat severe aortic valve disease. We hereby describe a novel case of RAVCAB performed via a single right lateral minimally invasive transaxillary approach.”
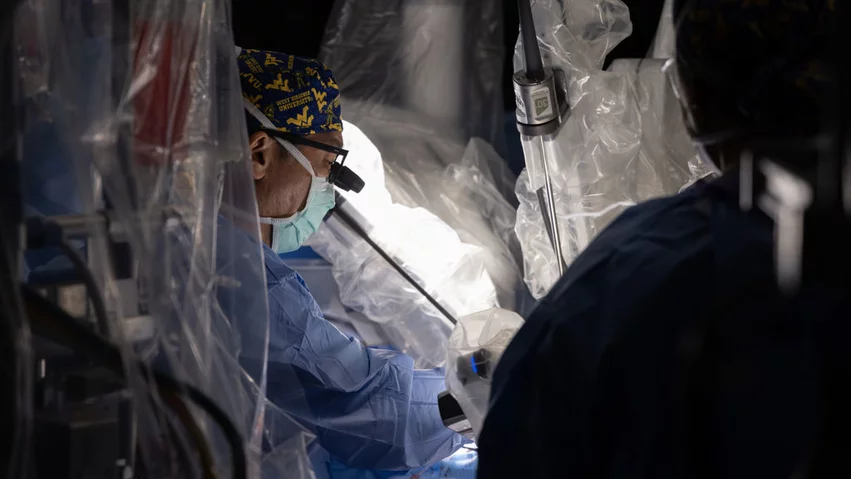
Badhwar et al. performed multiple test runs on cadavers to help prepare for the first-of-its-kind procedure. The team used its previous experience with RAVR as guidance to develop new techniques for left internal thoracic artery (LITA) harvest, LAD exposure and TECAB that could all be performed through a single incision on the far right of the patient’s chest.
When a 73-year-old female patient with a history of stroke, brain surgery and ongoing weight loss was first referred to Badhwar for treatment, her symptoms did not subside after six weeks of medical therapy. Badhwar’s team recommended open-heart surgery, but the patient and her family inquired about the potential of a less invasive treatment option. The care team then offered RAVCAB as a potential option, making it clear that she would be the first patient to every undergo such a procedure. If any issues occurred, all parties agreed that open-heart surgery could be performed as back-up option.
Badhwar and his team performed the robotic procedure on Oct. 31. In its analysis of the experience, the group wrote about two “elements” that they encountered. First, the patient presented with a “surprisingly robust amount of epicardial adipose tissue,” adding a new level of complexity. Second, the patient did not tolerate ventilation without transient oxygen desaturation and cerebral oximetric desaturation.
The surgery, however, was still a success, with a total clamp time of 224 minutes and total cardiopulmonary bypass time of 352 minutes. Ejection fraction improved from 35% prior to treatment to 45% after treatment, and the patient “recovered expectantly from her fail preoperative state.” She was finally discharged with an ejection fraction of 50%.
“As transcatheter alternatives to the management of aortic valve disease continue to evolve in lower risk patients, the ability to offer non-sternotomy surgical options is becoming more relevant for balanced heart team consideration,” the authors wrote. “Recently, a propensity matched comparison of RAVR to TAVR revealed that in low to intermediate risk patients, RAVR was associated with superior short-term and one-year outcomes. Although understanding of concomitant or staged TAVR and percutaneous coronary intervention continues to evolve, the outcomes of surgical aortic valve replacement and coronary artery bypass provide the current gold standard for low to intermediate risk patients. As the transcatheter field evolves, we suggest the surgical field should follow suit to offer patients with balanced minimally invasive alternatives. If RAVCAB outcomes can replicate those of conventional surgical therapy, this may provide a viable alternative to open surgical and transcatheter options.”
Click here for prior Cardiovascular Business coverage about this procedure. In addition, an in-depth Q&A with Badhwar is available here.