Space travel disrupts normal rhythm in heart cells
Heart tissue samples that spent 30 days at the International Space Station (ISS) showed low gravity conditions in space weakened the tissues and disrupted their normal rhythmic beats when compared to earth-bound samples from the same source. The finding has implications for the cardiac health of astronauts on long duration space flights.
Johns Hopkins Medicine scientists sent 48 human bioengineered heart tissue samples aboard a SpaceX resupply missions to the ISS in 2020, and again in March 2023.
The researchers said the heart tissues “really don’t fare well in space." Over time, the tissues aboard the space station beat about half as strong as tissues from the same source kept on Earth. The findings expand what scientists know about low gravity’s potential effects on astronauts’ survival and health during long space missions that are planned for the moon starting next year, and possibly to Mars in the next decade. The study also serves as model for studying heart muscle aging and therapeutics on Earth.
A report of the scientists’ analysis of the tissues was published this week in the Proceedings of the National Academy of Sciences.[1]
Previous studies showed some astronauts return to Earth with age-related conditions, including reduced heart muscle function and arrhythmias, and that some, but not all, effects dissipate over time after their return. Scientists wanted to study these effects at a cellular and molecular level to find ways to keep astronauts safe during long space flights, explained project leader Deok-Ho Kim, PhD, a professor of biomedical engineering and medicine at the Johns Hopkins University School of Medicine.
To create the cardiac payload, scientist Jonathan Tsui, PhD, coaxed human induced pluripotent stem cells (iPSCs) to develop into heart muscle cells. Tsui, who was a PhD student in Kim's lab at the University of Washington, accompanied Kim as a postdoctoral fellow when Kim moved to The Johns Hopkins University in 2019. They continued the space biology research at Johns Hopkins.
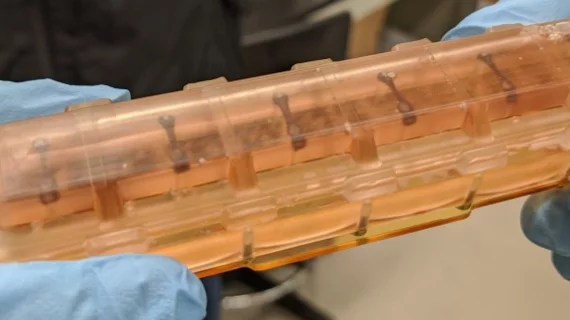
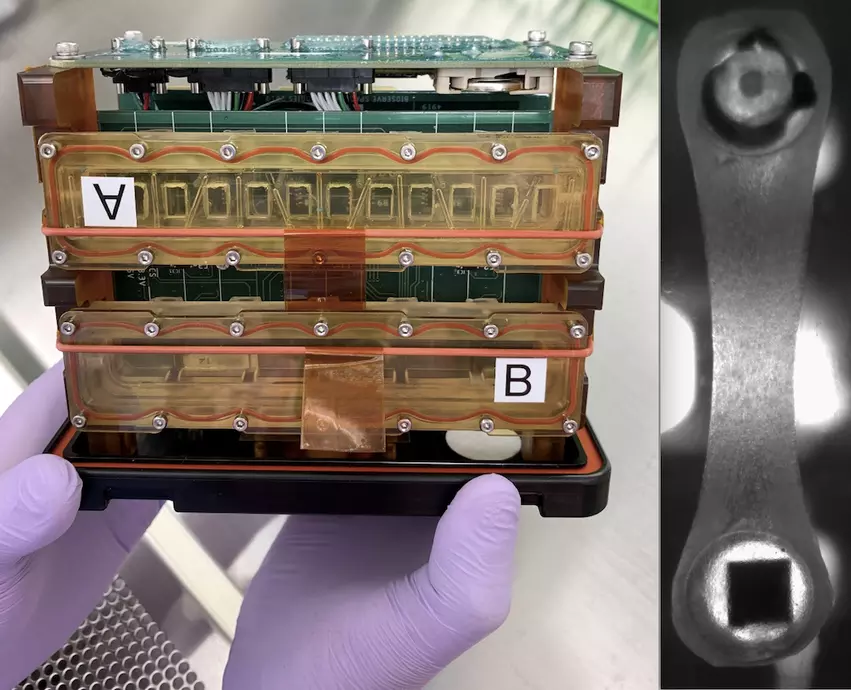
The tissues were placed in a bioengineered, miniaturized tissue chip that strings the tissues between two posts to collect data about how they contract. The cells’ 3D housing was designed to mimic the environment of an adult human heart in a chamber half the size of a cell phone. To get the tissues aboard the SpaceX CRS-20 mission in March 2020, Tsui said he had to hand carry the tissue chambers on a plane to Florida, and continue caring for the tissues for a month at the Kennedy Space Center before the launch. Tsui is now a scientist at Tenaya Therapeutics, a company focused on heart disease prevention and treatment.
NASA astronaut Kate Rubins conducts research for the Effect of Microgravity on Drug Responses Using Engineered Heart Tissues (Cardinal Heart) investigation onboard the International Space Station, one of several cardiovascular experiments on the ISS in recent years. Two more cardiac experiements launched to the ISS in March 2023. NASA Image
Once the tissues were on the space station, the scientists received real-time data for 10 seconds every 30 minutes about the cells’ strength of contraction, known as twitch forces, and on any irregular beating patterns. Astronaut Jessica Meir, PhD, MS, changed the liquid nutrients surrounding the tissues once each week and preserved tissues at specific intervals for later gene readout and imaging analyses.
The research team kept a set of cardiac tissues developed the same way on Earth, housed in the same type of chamber, for comparison with the tissues in space. When the tissue chambers from the ISS returned to Earth, Tsui continued to maintain and collect data from the tissues over time.
“An incredible amount of cutting-edge technology in the areas of stem cell and tissue engineering, biosensors and bioelectronics, and microfabrication went into ensuring the viability of these tissues in space,” Kim explained in a statement.
Key impacts of low gravity on the heart
In addition to losing strength, the heart muscle tissues in space developed arrythmias. Normally, the time between one beat of cardiac tissue and the next is about a second. This measure, in the tissues aboard the space station, grew to be nearly five times longer than those on Earth, although the time between beats returned nearly to normal when the tissues returned to Earth, the researchers said.
Sarcomeres, the protein bundles in muscle cells that help them contract, also became shorter and more disordered, which is a hallmark of human heart disease.
In addition, energy-producing mitochondria in the space-bound cells grew larger, rounder and lost the characteristic folds that help the cells use and produce energy.
The tissues from from space showed increased gene production involved in inflammation and oxidative damage, which are also hallmarks of heart disease.
“Many of these markers of oxidative damage and inflammation are consistently demonstrated in post flight checks of astronauts,” explained Devin Mair, PhD, a former student in Kim’s lab and now a postdoctoral fellow at Johns Hopkins.
Kim’s lab sent a second batch of 3D engineered heart tissues to the space station in 2023 to screen for drugs that may protect the cells from the effects of low gravity. This study is ongoing, and according to the scientists, these same drugs may help people maintain heart function as they get older.
Johns Hopkins Medicine researchers collaborating with NASA launched human heart “tissue-on-a-chip” specimens to the International Space Station (ISS) March 14. The cardiac myocytes will be monitored for impacts in pumping ability in the microgravity of space. Drugs will be tested o see if they improve pumping function. The right photo shows a closeup of the myocytes attached to two posts that measure contractility. Photos from Johns Hopkins
Impacts of cosmic radiation on the heart is the next frontier
The researchers at Hopkins are now using their tissue-on-a-chip system to study the effects of radiation on heart tissues at the NASA Space Radiation Laboratory. The ISS is in low Earth orbit, where the planet’s magnetic field shields occupants from most of the effects of space radiation. However, manned, long-duration missions to the moon and Mars will be outside the Earth's magnetic field. While we currently have the technology to fly to Mars or beyond, the big question is if astronauts could survive the journey.
Additional detailed data on what to expect from deep space travel radiation levels will be forthcoming from the unmanned Artemis I mission around the moon, which took place in late November-December 2022. To full-sized, medical-grade mannequin humans with thousands of radiation sensors to measure dosimetry for all organs in the body were strapped into the capsule to test how much radiation NASA astronauts will receive on future Artemis missions to the Moon. The complex human test phantoms were developed by CIRS and former American Association of Physicists in Medicine (AAPM) President Ehsan Samei, PhD, DABR, FAAPM, FSPIE, FAIMBE, FIOMP, FACR, chief imaging physicist for Duke University Health System and his team. Most of their research is geared toward measuring radiation precisely in studies for medical imaging and radiation therapy.
Read more about the radiation test equipment in the Artemis I mission.
Read more about this experiment in the article Heart tissue heads to space for research on aging and impact of long spaceflights.