Clinical decision support may improve cardiac care at low-income community health centers
A new study shows clinical decision support system (CDSS) software use was associated with significantly improved reversible risk of cardiovascular disease among socioeconomically vulnerable, high-risk patients. The study of more than 18,000 patients at community health centers (CHCs) was published Feb. 4 in the Journal of the American Medical Association.[1]
This cluster randomized clinical trial of 18,578 eligible patients by Kaiser Permanente found that although CDSS adoption rates are low, CDSS use was associated with significantly improved reversible risk of cardiovascular disease. The authors found clinical decision support needs to be used consistently to show benefit.
This cluster randomized clinical trial included 70 CHC clinics randomized to an intervention group (42 clinics; 8 organizations) or a control group that received no intervention (28 clinics; 7 organizations) from Sept. 20, 2018, to March 15, 2020. Patients aged 40 to 75 years with diabetes or atherosclerotic CVD and at least one uncontrolled major risk factor for cardiovascular disease (CVD), or a total reversible CVD risk of at least 10%, were the population targeted by the CDSS intervention.
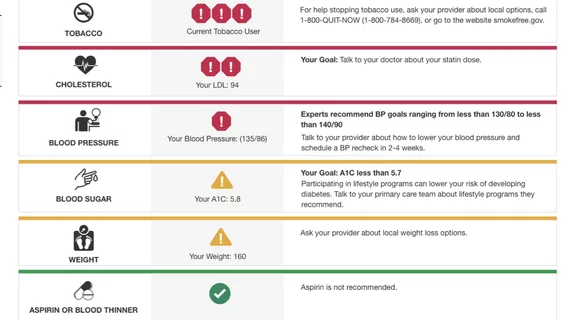
The point-of-care CDSS CV Wizard displayed real-time CVD risk factor control data and personalized, prioritized evidence-based care recommendations for each patient.
No population-level reduction in CVD risk was seen in patients in control or intervention clinics, but the mean reversible risk improved significantly more among patients in the control group over those at intervention clinics. However, when the CDSS was used, both risk measures decreased more among patients with high baseline risk in intervention than control clinics. The study's authors noted the mean reversible risk decreased by an absolute 4.4% among patients in intervention clinics compared with 2.7% among patients in control clinics.
Evidence-based management of modifiable risk factors for cardiovascular disease can substantially reduce CVD-related morbidity and mortality risks, the authors wrote. However, a deficit persists between recommended and observed CVD risk management, especially among vulnerable lower-income patients. One reason for this is that primary care clinicians must consider multiple factors affecting CVD risk for a given patient and determine which to address to optimally affect that patient’s risk within a brief encounter. Electronic health record–based CDSS address these barriers by alerting clinicians when patients have uncontrolled CVD risks and suggesting treatment options.
The technology used was the CV Wizard, a nonproprietary, web-based CDSS developed at HealthPartners Institute, a large, nonprofit, integrated healthcare system. The algorithms of the software reflect current CVD care guidelines and account for a patient’s blood pressure, laboratory results, distance from goals, medications, and comorbidities.
This study was supported by a National Institutes of Health (NIH) grant.
Reference: