CVIS: Improving Departments from Within
Cardiology departments are learning that their cardiovascular information systems (CVIS) are the perfect conduit to produce actionable and quantifiable data that can drive quality process improvement and cost savings.
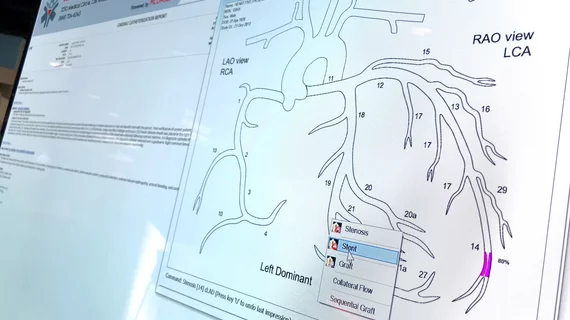
Quality measures can easily be measured from CVIS data
Properly utilizing and disseminating data gathered from a CVIS requires a systematic approach that should extend throughout a healthcare network, says Mark Watts, system imaging manager for Iasis Healthcare’s 16 hospitals in six U.S. states. The deployment of a widespread IT project needs complete administrative support, and should be bolstered and reviewed by a physician champion.
Watts installed a CVIS at his previous employer, Provena Healthcare, a six-hospital system in Illinois, and currently is undertaking a similar, larger scale implementation with Horizon Cardiology CVIS (McKesson) at Iasis’ facilities. Once deployed, hundreds of reports can be acquired via the CVIS, and these data can be mined to help improve myriad processes and quality initiatives.
Methodist DeBakey Heart & Vascular Center in Houston was an early adopter of CVIS when in 2003 it implemented a Digisonics system, says Director Marti L. McCulloch. The center has 10 operating rooms, eight cath labs, 154 acute-care beds, 48 ICU beds and 30 transplant beds.
Methodist tracks quality measures, such as study turnaround times and patient report turnaround times, which can be pulled from the database to assess physician performance. Then, the provider disseminates the data through a quality metrics dashboard. “Regardless of the superiority of the clinicians or their interpretation, if the report doesn’t get sent off to the referring physician in a timely manner, its relevance is lost,” says McCulloch.
When the CVIS was first installed, the facility discovered its vascular lab had an average report turnaround time of 10-plus days. The average turnaround time now is 24 hours.
Barry Szakolczay, data specialist for the cardiovascular services at Scottsdale Healthcare, a three-hospital network with about 850 beds in Scottsdale, Ariz., says the institution generates between 70 and 90 reports monthly from the CVIS. Scottsdale Healthcare went live with its Centricity DMS (GE Healthcare) in late 2006.
Scottsdale Healthcare frequently monitors length of stay for the cath lab and cardiac surgery. With those data, length of stay from admission to procedure, length of stay from procedure to discharge and total length of stay can be reviewed by cardiologists and cardiovascular surgeons. Surgery data are entered into the Adult Cardiac Registry of the Society of Thoracic Surgery (STS), allowing the society to evaluate outcomes on a national level. One of the key data elements the society tracks is patients with a hospital length of longer than 14 days. Data collected in the cath labs also are entered into an American College of Cardiology (ACC) registry, allowing the provider to compare outcomes nationally.
“If a surgical patient had an extended stay of 14 days or beyond, our surgeons would review that case to assess why the patient stay was prolonged. The only way we are able to track these factors on a frequent basis is through reports issued from the DMS,” Szakolczay says.
Patient outcomes data more easily accessed on CVIS
Scottsdale Healthcare’s CVIS has a statistical risk report which extracts data from an STS module, and examines the outcome/expected outcome ratio of patients for such events as mortality, renal failure, re-op, prolonged ventilation and deep sternal wound infection rate. Patient characteristics and co-morbidities also are available from the database. The STS module assigns a risk score to each patient for each of the categories, and that information is pulled onto a report from the CVIS. Biannually, Szakolczay and his colleagues meet with the surgeons to review expected outcomes, compared with actual outcomes.
Szakolczay says that the “surgeons rely on these data very heavily, and look forward to seeing the report and where they stand, as well as where they can make improvements.”
Likewise, at Iaisis Healthcare, the CVIS produces “hard facts that allow managers to have serious, productive conversations with their physicians, who in turn, have tremendous clout within the community and within the organization,” Watts says. Within the cath lab, there has been a tremendous push to reduce door-to-balloon times.
For the ACC/AHA databases on door-to-balloon times, figures can be captured in real-time via hemodynamic equipment and fed back into the CVIS while the case is ongoing. The report also can indicate when the ED calls the cath lab, ED triage times, the time of the first EKG, when the cardiologist was called, when the patient arrived at the cath lab and when the first balloon was inflated.
“These different times are captured in the CVIS report, indicating which areas need improvement, and therefore, have helped facilities greatly improve door-to-balloon times,” Szakolczay says. “In fact, any case that takes longer than 90 minutes is reviewed at Scottsdale to determine where the delay occurs.”
J. Brent Muhlestein, MD, professor of medicine at the J. L. Sorenson Heart & Lung Center, Intermountain Medical Center in Murray, Utah, also speaks to the importance of CVIS data in tailoring procedures to produce the best outcomes for patients. Muhlestein and his colleagues have been conducting small trials to determine best practices based on CVIS data from across Intermountain’s 21 hospitals.
For example, Muhlestein uses the CVIS to help determine which anticoagulants are beneficial in the cath lab based on risks associated with bleeding and ischemic complications. Using these data, “we were able to more effectively define our institution’s protocols, and also publish our findings in journal articles to disseminate the information to other departments.” Based on data from the CVIS, Muhlestein and colleagues were able to show that bleeding risks associated with glycoprotein IIb/IIIa inhibitors are significantly reduced, if the heparin dose is reduced.
Cost savings of using a CVIS
To monitor expenses, Scottsdale Healthcare issues a monthly inventory report via the CVIS to its cath lab supervisors. In addition, Szakolczay runs a weekly device implant report for electrophysiology, assessing how many devices are being used, from which vendor and which percentage of the hospital’s market share they are consuming. That report gets issued to the director of the cardiovascular service line, as well as to the medical director for electrophysiology. Then, on a monthly basis, a similar report is distributed to the cath lab managers and supervisors and contract management. “This information allows contract management to negotiate better prices with the vendors,” Szakolczay says. “The report plays a big part in negotiations and keeping contract management abreast of what is being used, and therefore saves on the bottom line.”
Muhlestein and his colleagues use CVIS data to determine outcomes of bare-metal and drug-eluting stents, and having found very few different outcomes among the various brands, the managers negotiated better prices based on their clinical outcomes.
Watts agrees that inventory management through CVIS reports has been a major source of cost savings. For example, data can be collected on stenting procedures performed by 40 different cardiologists. The resulting data indicate an average 2.2 stents are used during each procedure. “Overall, this isn’t an alarming figure, but when those data are drilled down per stent, per physician or whether the case was planned or emergent, then department managers can begin to evaluate physician practices which could be costing the department unnecessary expenses,” he says.