5 key takeaways from new ACC/AHA aortic disease guidelines
The American College of Cardiology (ACC) and American Heart Association (AHA) have released new guidelines for the diagnosis and management of patients presenting with aortic disease. The in-depth document, published in the Journal of the American College of Cardiology, covers a variety of topics, including thoracic aortic disease, peripheral artery disease, shared decision-making and cardiac imaging.[1]
“There has been a host of new evidence-based research available for clinicians in the past decade when it comes to aortic disease,” writing committee chair Eric M. Isselbacher, MD, MSc, a cardiologist with Massachusetts General Hospital, said in a prepared statement. “It was time to re-evaluate and update the previous, existing guidelines. We hope this new guideline can inform clinical practices with up-to-date and synthesized recommendations, targeted toward a full multidisciplinary aortic team working to provide the best possible care for this vulnerable patient population.”
These are 5 key takeaways from the new recommendations:
1. Updated definitions: Clinicians cannot diagnose or manage aortic disease if they do not know the basics
The ACC/AHA recommendations begin with a thorough rundown of the standard aortic anatomy. When you are focusing on the largest artery in the human body, it is important to know every detail about its composition and segmentation. Thoracic and abdominal aorta landing zones are also covered in great detail, which is vital information when it comes to performing certain endovascular procedures. Arterial aneurysms, aortic dissections, intramural hematomas and many more concepts are also defined and explained at the beginning of the document.
2. Medical imaging plays a key role in the diagnosis and management of aortic disease
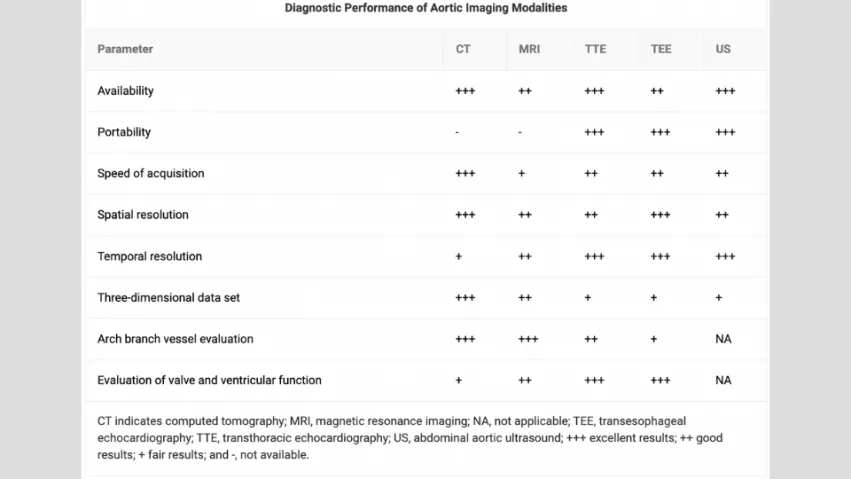
All cardiac imaging, including CT, MRI and echocardiography exams, should use standardized acquisition and measurement techniques on a consistent basis. Ionizing radiation should be kept to a minimum.
The ACC/AHA recommendations also compare the diagnostic performance of these different modalities with a graphic. Transthoracic echocardiograms (TTEs) and ultrasounds, for example, earn the high marks for their portability. Cardiac MRIs, meanwhile, earn high marks for their arch branch vessel evaluation capabilities.
3. Multidisciplinary teams can provide significant value in aortic assessments
Whenever possible, multidisciplinary teams should determine the next steps for patients with acute aortic disease who may require an urgent repair.
“Evidence-based standards for medical and surgical conditions recognize the critical relationship among both hospital and surgeon case volumes and patient outcomes,” according to the ACC/AHA recommendations. “Clinical excellence is further enhanced by collaborative, multispecialty teams to foster the best treatment of patients, especially for complex presentations with multiorgan threats. Although there is no agreed-on definition of a multidisciplinary aortic team, an appropriate framework might be: A specialized hospital team with an exceptionally high concentration of expertise in the evaluation and management of aortic disease, in which care is delivered in a comprehensive, multidisciplinary manner.”
On a related note, referring patients to high-volume surgical centers may be necessary, especially if they present with multiple chronic conditions.
4. Shared decision-making is recommended, especially when the patient is pregnant or may be considering pregnancy
Patients and their families should be involved in the decision-making process when possible. The use of decision aids is encouraged to help patients understand the different options available to them.
“Shared decision-making is especially useful when considering the diameter thresholds for and the timing of intervention in addition to having an important role in considering the risks of pregnancy in patients with underlying aortic disease,” according to the ACC/AHA recommendations.
5. Aortic recommendations evolve over time
One key purpose of this document is to update clinicians about certain recommendations that have changed over the years. For example, the threshold for the surgical intervention in patients with sporadic aortic root and ascending aortic aneurysms has been lowered from 5.5 cm to 5 cm if a multidisciplinary aortic team is available. In some high-risk patients facing certain scenarios, the threshold may be even lower.
These points are just the tip of the iceberg. The full document is available here.
More at AHA Scientific Sessions 2022
These guidelines will also be the topic of a presentation, “Highlights of the New AHA/ACC Aortic Disease Guidelines,” on Nov. 7 at the AHA Scientific Sessions 2022 conference in Chicago. Isselbacher is scheduled to lead the presentation. More information is available here.
Stay tuned to Cardiovascular Business for additional coverage of the conference, including breaking news and exclusive interviews. Read through the conference’s late-breaking studies here.